Predicting the Safe Use of Deceased after Circulatory Death Liver Allografts in Primary Sclerosing Cholangitis
Department of Transplantation, University of Wisconsin, Madison, WI
Meeting: 2020 American Transplant Congress
Abstract number: D-132
Keywords: Donors, non-heart-beating, Liver transplantation, Resource utilization
Session Information
Session Name: Poster Session D: Liver: Recipient Selection
Session Type: Poster Session
Date: Saturday, May 30, 2020
Session Time: 3:15pm-4:00pm
 Presentation Time: 3:30pm-4:00pm
Presentation Time: 3:30pm-4:00pm
Location: Virtual
*Purpose: The use of deceased after circulatory donation (DCD) liver allografts in patients with primary sclerosing cholangitis (PSC) is controversial given the already-increased risk of bile duct complications in PSC patients. We hypothesized that DCD organs appropriately matched to patients with PSC using the UK DCD scoring system (UKSS) are not associated with increased risk of graft failure or mortality.
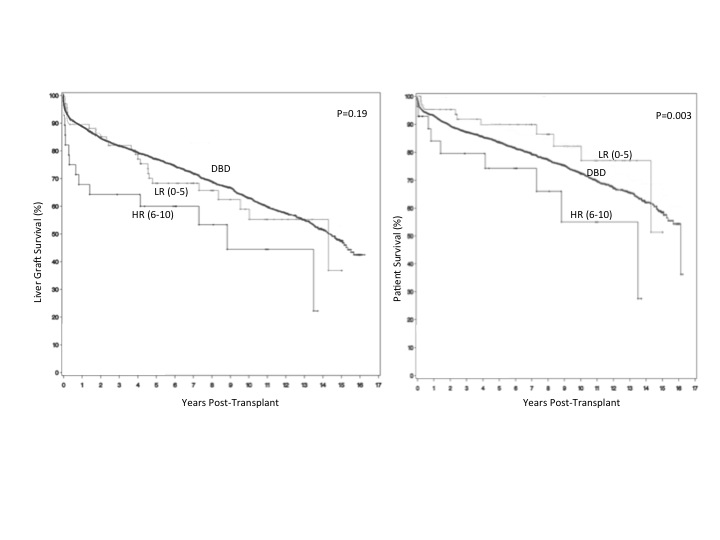
*Methods: We analyzed 99,229 transplants in the OPTN database from 1/2001 to 3/2015. Endpoints were graft failure and mortality. Results were controlled for donor and recipient demographics; share type; and cold- (CIT) and functional warm-ischemic time (fWIT). Statistical analysis utilized chi-square, Cox proportional hazards, and Kaplan-meier plots in SAS. DCD transplants were stratified by UKSS low-risk (LR, score ≤5) or high-risk (HR, 6-10).
*Results: 3,958 PSC patients undergoing DBD transplantation (PSC-DBD) and 95 PSC-DCD were identified. DCD donors were younger than DBD (33.1 vs. 40.7), more commonly male (66.1% vs. 57.7%) and more commonly Caucasian (90.4% vs. 71.6%). Recipient demographics were similar between DBD and DCD. Average 5-year graft survival was lower in DCD than DBD recipients (69.0% DCD vs. 78.4% DBD, p=0.02). When stratified according to the UKSS, the LR group had a5-year graft survival similar to the DBD group (78.4% DBD vs. 75.4% LR, p=0.52) but significantly higher than in the HR group (75.4% LR vs. 60.0% HR, p=0.02). On multivariate analysis, the LR group had statistically equivalent graft survival to the DBD group (OR 1.23, p=0.31), but the HR group had a significantly increased risk of graft loss (OR 1.92, p=0.01). Patient survival at 5 years was higher in the LR than the HR group (89.9% vs. 74.3%, p=0.02) but UKSS score did not correlate with increased mortality on multivariate analysis (p=0.42).
*Conclusions: Graft failure is significantly higher in PSC-DCD recipients compared to receiving a DBD; however, the risk of graft loss is abrogated by using appropriately-matched donor and recipient combinations to create a UKSS low-risk score. Given the high waitlist mortality of patients with PSC, DCD donors should be considered a viable organ source for these patients.
To cite this abstract in AMA style:
Fleetwood V, Gracon A, Aufhauser D, Papageorge C, Janek K, Leverson G, Foley D, Mezrich J, D'Alessandro A, Fernandez L, Al-Adra D. Predicting the Safe Use of Deceased after Circulatory Death Liver Allografts in Primary Sclerosing Cholangitis [abstract]. Am J Transplant. 2020; 20 (suppl 3). https://atcmeetingabstracts.com/abstract/predicting-the-safe-use-of-deceased-after-circulatory-death-liver-allografts-in-primary-sclerosing-cholangitis/. Accessed February 22, 2026.« Back to 2020 American Transplant Congress