Postoperative Renal Function Predicts Length of Stay for Incisional Hernia Repair after Liver Transplantation
Transplant Surgery, Indiana University, Indianapolis, IN.
Meeting: 2018 American Transplant Congress
Abstract number: D255
Keywords: Length of stay, Liver, Renal dysfunction
Session Information
Session Name: Poster Session D: Surgical Issues (Open, Minimally Invasive): All Organs
Session Type: Poster Session
Date: Tuesday, June 5, 2018
Session Time: 6:00pm-7:00pm
 Presentation Time: 6:00pm-7:00pm
Presentation Time: 6:00pm-7:00pm
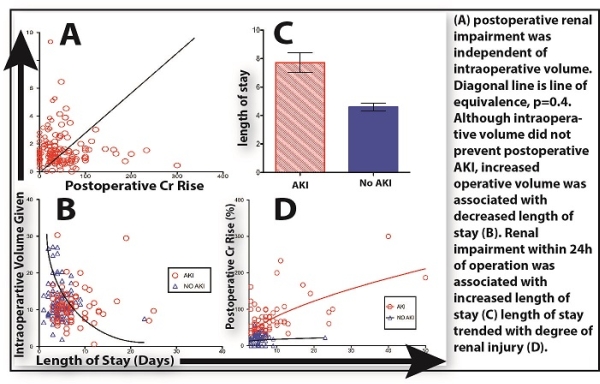
Location: Hall 4EF
Background: Incisional hernia repair (IHR) is the most frequently performed general surgery procedure after orthotopic liver transplantation (OLT). Although enhanced recovery protocols for general surgery are increasingly favored, the post-OLT patient may not benefit from all aspects of these models. The aims of the present study is to describe variables that affect length of stay for this unique population. Methods: We conducted a retrospective review upon a series of adult patients undergoing IHR after OLT at a single center between 2005 and 2016. Primary endpoint was length of stay. Results were stratified by demographic, intraoperative, and postoperative variables. Results: From a population of 1,954 patients undergoing OLT, 172 patients (11.3%) subsequently underwent IHR during the years 2005 to 2016. The median length of stay was 5 day (range 2-50). Operative time, thoracic epidural catheters, increased BMI, and lower preoperative albumin were associated with increased length of stay. The strongest predictor of length of stay was postoperative renal function. Despite liberal intraoperative volume administration (median 642 ml/hr) and brisk intraoperative urine output (median 72ml/hr), postoperative AKI occurred in 48% of patients (Figure 1A). Although all patients returned to their baseline Cr by discharge, postoperative renal impairment had a significant impact on length of stay (Figure 1B-D). Conclusions: In patients undergoing IHR after OLT, immediate postoperative renal function is decreased independent of intraoperative venous preload. Likely owed to the enterohepatic circulation of nephrotoxic immunosuppression, this offers an important consideration for OLT patients undergoing general surgery. Although many aspects of current ERAS protocols may be applied to post-transplant patients, intraoperative volume should not be restricted in this patient population.
CITATION INFORMATION: Butler J., O'Brien D., Kays J., Kubal C., Ekser B., Fridell J., Mangus R., Powelson J. Postoperative Renal Function Predicts Length of Stay for Incisional Hernia Repair after Liver Transplantation Am J Transplant. 2017;17 (suppl 3).
To cite this abstract in AMA style:
Butler J, O'Brien D, Kays J, Kubal C, Ekser B, Fridell J, Mangus R, Powelson J. Postoperative Renal Function Predicts Length of Stay for Incisional Hernia Repair after Liver Transplantation [abstract]. https://atcmeetingabstracts.com/abstract/postoperative-renal-function-predicts-length-of-stay-for-incisional-hernia-repair-after-liver-transplantation/. Accessed February 20, 2026.« Back to 2018 American Transplant Congress