Post-Transplant Reduction in Pre-Existing Donor-Specific Antibody Levels After Belatacept- vs Cyclosporine-Based Immunosuppression.
1Emory University, Atlanta, GA
2Bristol-Myers Squibb, Lawrenceville, NJ
Meeting: 2017 American Transplant Congress
Abstract number: 169
Keywords: Antibodies, Donors, HLA antibodies, Kidney transplantation, marginal
Session Information
Session Name: Concurrent Session: Novel Immunosuppression - DSA Monitoring
Session Type: Concurrent Session
Date: Sunday, April 30, 2017
Session Time: 4:30pm-6:00pm
 Presentation Time: 5:06pm-5:18pm
Presentation Time: 5:06pm-5:18pm
Location: E450b
Purpose: We explored the effect of belatacept (bela)- and cyclosporine (CsA)-based immunosuppression (IS) on pre-existing donor-specific antibody (DSA) levels by mean fluorescence intensity (MFI) in patients (pts) enrolled to BENEFIT and BENEFIT-EXT.
Methods: In both studies, T-cell–negative crossmatch kidney transplant recipients were randomized to bela more intense (MI)-, bela less intense (LI)-, or CsA-based IS. Pre-existing DSAs were assessed centrally at baseline via solid phase flow cytometry. Samples from DSA-positive pts were tested with Luminex single-antigen bead assays.
Results: In BENEFIT, pre-existing DSAs were detected in 4.6%, 4.9%, and 6.8% of pts randomized to bela MI, bela LI, and CsA, respectively. In BENEFIT-EXT, these values were 6.5%, 5.7%, and 9.2%, respectively. The HLA class distribution of DSAs by treatment arm was similar in each study.
| BENEFIT | BENEFIT-EXT | |||||
| Bela MI
(n=10) |
Bela LI
(n=11) |
CsA
(n=15) |
Bela MI
(n=12) |
Bela LI
(n=10) |
CsA
(n=17) |
|
| Mean age, y | 49.6 | 45.0 | 44.1 | 55.2 | 53.8 | 57.7 |
| Antibody class, n (%)
I II Both |
7 (70)
2 (20) 1 (10) |
7 (64)
3 (27) 1 (9) |
10 (67)
4 (27) 1 (7) |
9 (75)
2 (17) 1 (8) |
7 (70)
2 (20) 1 (10) |
12 (71)
2 (12) 3 (18) |
| PRA, n (%)
<20% ≥20% Missing |
7 (70)
1 (10) 2 (20) |
4 (36)
3 (27) 4 (36) |
6 (40)
5 (33) 4 (27) |
12 (100)
0 (0) 0 (0) |
8 (80)
1 (10) 1 (10) |
14 (82)
2 (12) 1 (6) |
In both studies, more pts assigned to bela MI had baseline PRA <20% than ≥20%. Over the first 2 years, bela-treated pts exhibited greater decreases in DSA MFI vs CsA-treated pts.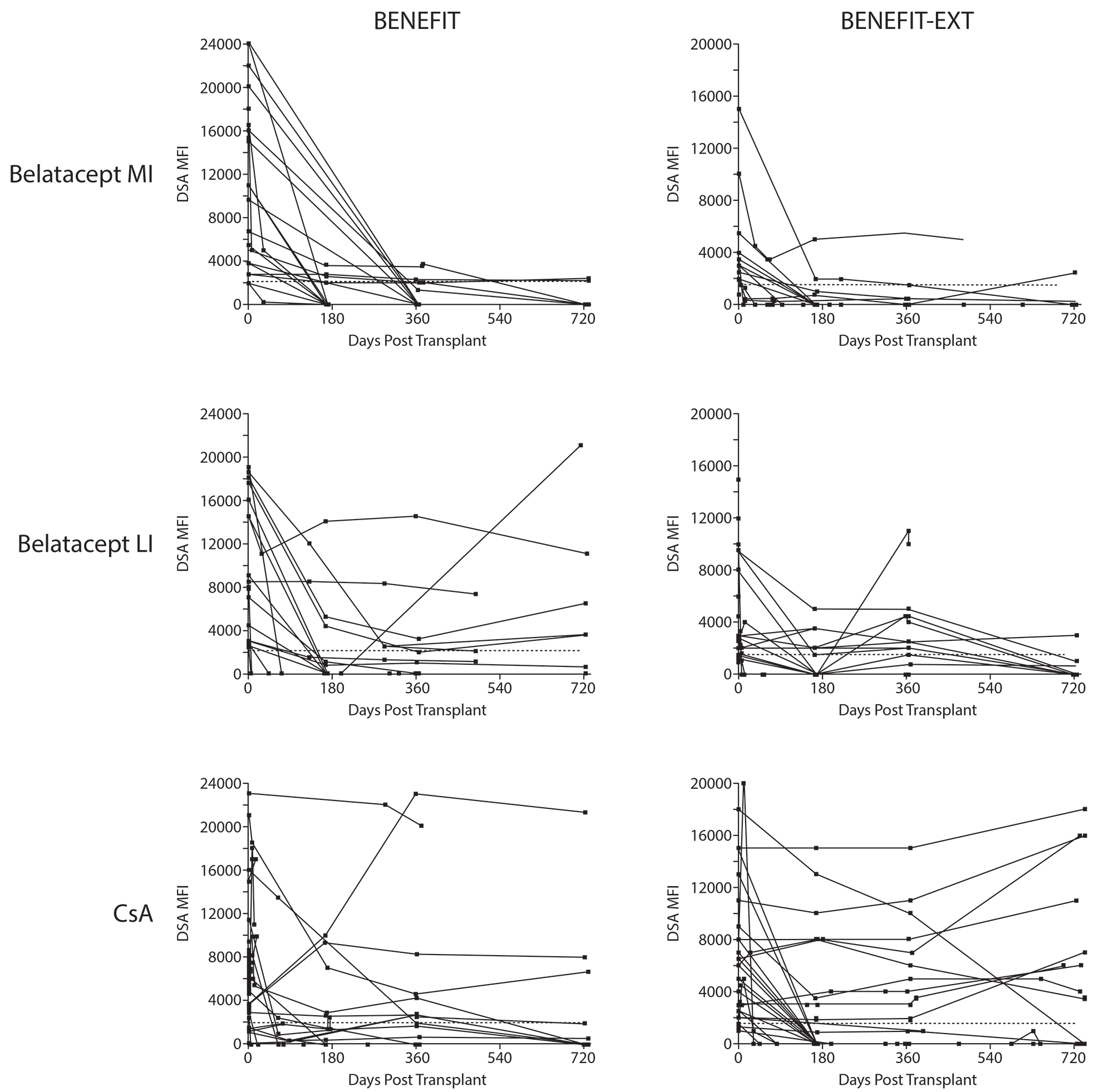 The effect of bela-based IS on DSA levels was more pronounced in BENEFIT-EXT vs BENEFIT. In both studies, MFI decline was more apparent with bela MI vs bela LI. Total IgG, IgM, and IgA levels were also reduced in bela-treated pts. Due to small sample sizes, clinical outcomes were not assessed.
The effect of bela-based IS on DSA levels was more pronounced in BENEFIT-EXT vs BENEFIT. In both studies, MFI decline was more apparent with bela MI vs bela LI. Total IgG, IgM, and IgA levels were also reduced in bela-treated pts. Due to small sample sizes, clinical outcomes were not assessed.
Conclusions: Bela-based IS leads to greater decreases in DSA MFI in pts with pre-existing DSAs vs CsA-based IS.
CITATION INFORMATION: Bray R, Gebel H, Townsend R, Polinsky M, Yang L, Meier-Kriesche U, Larsen C. Post-Transplant Reduction in Pre-Existing Donor-Specific Antibody Levels After Belatacept- vs Cyclosporine-Based Immunosuppression. Am J Transplant. 2017;17 (suppl 3).
To cite this abstract in AMA style:
Bray R, Gebel H, Townsend R, Polinsky M, Yang L, Meier-Kriesche U, Larsen C. Post-Transplant Reduction in Pre-Existing Donor-Specific Antibody Levels After Belatacept- vs Cyclosporine-Based Immunosuppression. [abstract]. Am J Transplant. 2017; 17 (suppl 3). https://atcmeetingabstracts.com/abstract/post-transplant-reduction-in-pre-existing-donor-specific-antibody-levels-after-belatacept-vs-cyclosporine-based-immunosuppression/. Accessed February 17, 2026.« Back to 2017 American Transplant Congress
