Phenotype and Outcome of Antibody-Mediated Rejection Due to Pre-Existing and De Novo DSA in Kidney Recipients.
1Paris Research Center for Organ Transplantation, Paris, France
2University of Alberta, Edmonton, Canada
3ATAGC, Edmonton, Canada.
Meeting: 2016 American Transplant Congress
Abstract number: 278
Keywords: Graft survival, Kidney transplantation, Rejection
Session Information
Session Name: Concurrent Session: Antibody Mediated Rejection in Kidney Transplantation: De Novo DSA
Session Type: Concurrent Session
Date: Monday, June 13, 2016
Session Time: 4:30pm-6:00pm
 Presentation Time: 4:54pm-5:06pm
Presentation Time: 4:54pm-5:06pm
Location: Ballroom B
Antibody-mediated rejection (ABMR) presents with either pre-existing or de novo DSA. The aim of the study was to compare the two ABMR phenotypes and their outcome. From a cohort of 965 kidney biopsies from two North American and five European centers, we selected all patients with ABMR. In 205 patients with ABMR, 101 (49%) had pre-existing DSA and 104 (51%) de novo DSA. The median time from transplantation to biopsy-proven ABMR (TxBx) was earlier with pre-existing DSA (2.8 months) compared to de novo DSA (3.9 years). There was no difference for the GFR: 39.3 mL/min/1.73m2 for pre-existing DSA vs 41.3 for de novo DSA (p=0.487) but the de novo DSA group had more proteinuria (1.5 vs. 0.5 g/g creatinine) (p<0.001). Kidney biopsies with pre-existing DSA presented with more glomerulitis (mean g score 1.73 vs. 1.05), less transplant glomerulopathy (0.48 vs. 1.27) but similar peritubular capillaritis and C4d deposition. ABMR with pre-existing DSA more often had Class I DSA (40% vs. 25%, p=0.018) but lower mean MFI (5096 vs. 8587, p=0.002). Using the gene expression assessment, ABMR with pre-existing DSA exhibited more injury-repair response associated transcripts (IRRATS) (p=0.008) but less Gamma interferon inducible transcripts (GRIT1), NK cell transcript burden (NKB) and T cell transcript burden (TCB) (p=0.018, p=0.010 and p<0.001). The two ABMR phenotypes exhibited similar endothelial cell-associated transcript (ENDAT) expression and ABMR scores. Kidney allograft survival at 4 and 8 years after rejection was superior in the pre-existing DSA phenotype (78% and 63%) compared to the de novo DSA phenotype (54% and 35%) (p<0.001). Using a random forest, the most important variables associated with graft survival were GFR, proteinuria, TxBx, and the ABMR phenotype. Thus early ABMR with pre-existing DSA is associated with better allograft survival compared to late ABMR with de novo DSA. Among the potential explanations for superior results with early ABMR with pre-existing DSA are the aggressive early detection and treatment protocols used for this phenotype.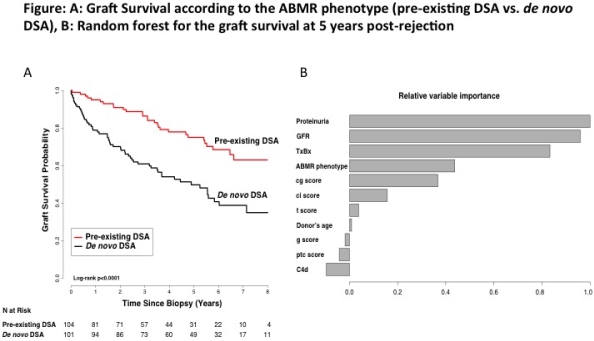
CITATION INFORMATION: Aubert O, Loupy A, Hidalgo L, Reeve J, Glotz D, Legendre C, Lefaucheur C, Halloran P. Phenotype and Outcome of Antibody-Mediated Rejection Due to Pre-Existing and De Novo DSA in Kidney Recipients. Am J Transplant. 2016;16 (suppl 3).
To cite this abstract in AMA style:
Aubert O, Loupy A, Hidalgo L, Reeve J, Glotz D, Legendre C, Lefaucheur C, Halloran P. Phenotype and Outcome of Antibody-Mediated Rejection Due to Pre-Existing and De Novo DSA in Kidney Recipients. [abstract]. Am J Transplant. 2016; 16 (suppl 3). https://atcmeetingabstracts.com/abstract/phenotype-and-outcome-of-antibody-mediated-rejection-due-to-pre-existing-and-de-novo-dsa-in-kidney-recipients/. Accessed February 25, 2026.« Back to 2016 American Transplant Congress
