Pharmacist-Led Renal-Sparing Conversion to Everolimus After Liver Transplantation
1Barnes-Jewish Hospital, St. Louis, MO
2Washington University in St. Louis, St. Louis, MO.
Meeting: 2015 American Transplant Congress
Abstract number: A209
Keywords: Immunosuppression, Liver transplantation, Renal function
Session Information
Session Name: Poster Session A: Liver: Immunosuppression and Rejection
Session Type: Poster Session
Date: Saturday, May 2, 2015
Session Time: 5:30pm-7:30pm
 Presentation Time: 5:30pm-7:30pm
Presentation Time: 5:30pm-7:30pm
Location: Exhibit Hall E
Purpose: Preservation of renal function following orthotopic liver transplantation (OLT) through calcineurin inhibitor (CNI)-minimization is an established clinical objective. The use of everolimus (EVR) to reduce tacrolimus (TAC) exposure was recently shown to provide superior renal function 36 months post-OLT compared with patients on standard TAC therapy.
Methods: We performed a retrospective cohort study of adult OLT recipients transplanted since 2013 who were placed on a CNI-minimization regimen (TAC trough goal 3-5 ng/mL) with EVR (goal trough 3-8 ng/mL). Clinical pharmacists prospectively identified patients based on eGFR (30-70 mL/min), absence of proteinuria (urine protein <500mg/day), total cholesterol <350 mg/dL, and fasting triglycerides <500 ng/dL. The primary endpoint was the change in renal function from CNI-minimization, as assessed by eGFR at 4, 12, and 24 weeks post-conversion. Renal function was compared with a cohort of patients meeting the same criteria, who remained on standard TAC therapy (goal trough 6-10 mg/mL).
Results: In total, 42 patients met criteria and were converted to EVR, and were compared to 42 control patients. There were no differences in race, sex, CMV risk, hepatocellular carcinoma or primary diagnoses between groups, however 4 patients in the control arm had a rejection. MELD, cold ischemic time, and creatinine at transplant were well-matched. Median time to conversion was 108 days, and this was used as reference time in the control arm. Baseline mean eGFR was similar across arms (58.6 vs. 57.3 mL/min, p = 0.665) 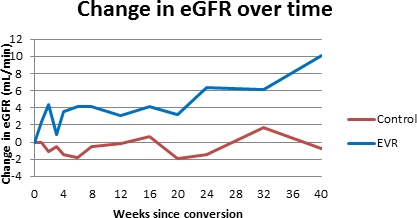 There was a significantly higher mean change in eGFR in week 4, week 12 and week 24 in the EVR conversion arm (-1.5 mL/min in the control arm vs +6.4 mL/min in the EVR arm, p = 0.029). No treatment-limiting adverse events occurred in either group through 24 weeks of follow-up.
There was a significantly higher mean change in eGFR in week 4, week 12 and week 24 in the EVR conversion arm (-1.5 mL/min in the control arm vs +6.4 mL/min in the EVR arm, p = 0.029). No treatment-limiting adverse events occurred in either group through 24 weeks of follow-up.
Conclusion: We note a significant improvement in renal function for patients on EVR compared to those on standard TAC, demonstrating successful implementation of a pharmacist-driven CNI-minimization strategy following OLT.
To cite this abstract in AMA style:
Horwedel T, Bowman L, Chapman W, Hagopian J. Pharmacist-Led Renal-Sparing Conversion to Everolimus After Liver Transplantation [abstract]. Am J Transplant. 2015; 15 (suppl 3). https://atcmeetingabstracts.com/abstract/pharmacist-led-renal-sparing-conversion-to-everolimus-after-liver-transplantation/. Accessed March 6, 2026.« Back to 2015 American Transplant Congress
