Personalized Medicine Using Next-Generation Sequence for Kidney Transplant Recipients
Intermountain Medical Center, Murray, UT
Meeting: 2022 American Transplant Congress
Abstract number: 1415
Keywords: Genomics, Kidney, Screening
Topic: Clinical Science » Kidney » 49 - Recurrent Kidney Disease & Genetics
Session Information
Session Name: Recurrent Kidney Disease & Genetics
Session Type: Poster Abstract
Date: Monday, June 6, 2022
Session Time: 7:00pm-8:00pm
 Presentation Time: 7:00pm-8:00pm
Presentation Time: 7:00pm-8:00pm
Location: Hynes Halls C & D
*Purpose: Tissue diagnosis definitely drives therapeutic and prognostic decisions amongst patients with chronic kidney disease (CKD). However, patients with CKD often present late in the course, when kidney biopsy is not a viable option. We hypothesized that genetic screening for kidney diseases in patients presenting for transplant evaluation without a tissue/certain clinical diagnosis would refine their diagnosis, screen for recurrence prone diseases and bear therapeutic implications.
*Methods: Transplant recipients with unknown clinical/pathological diagnosis were included. We utilized Renasight™(Natera), which provides analysis on 382 genes associated with kidney disease.
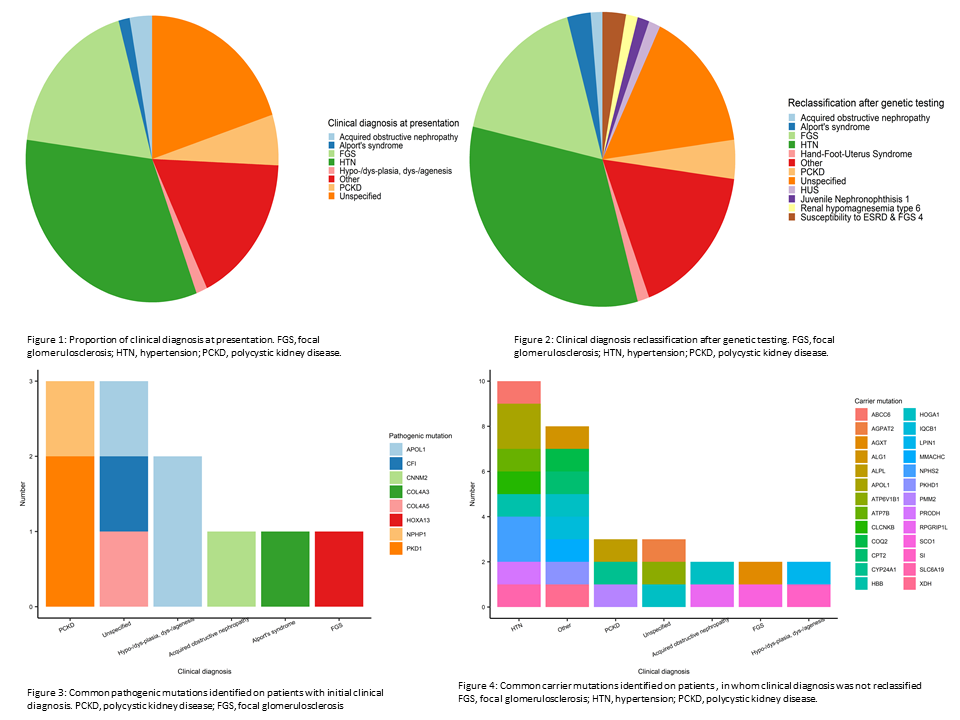
*Results: A total of 70 patients were included from July 2020 to June 2021. 37.1% patients were females with median age was 50 years. Population demographics were as follows: Caucasian (41.4%), Hispanics (20%); clinical diagnosis at presentation- hypertension (32.9%), unspecified (20%), and Focal Glomerulosclerosis (FGS) (18.6%). Genetic testing identified positive mutation in ten patients. It reclassified eight patients (11.4%) in the following diagnostic categories: two patients as susceptibility to ESRD (end stage renal disease) and FGS; two patient as Alport’s Syndrome; one patient as Renal hypomagnesemia type 6; one patient as Juvenile Nephronophthisis 1; one patient with Hemolytic uremic Syndrome (HUS) with CFI mutation; and one patient with Hand-Foot-Uterus Syndrome (Figure 1). Two additional patients with know Polycystic Kidney Disease (PCKD) were screened due to other associated clinical phenotype, and were found to be positive for PKD1, as expected (Figure 1). The common pathogenic mutations identified in the above patients, classified based on clinical diagnosis at presentation has been shown in Figure 2-A, which bore implications on reclassifications. Additional carrier mutations found in patients who were not reclassified, are shown in Figure 2- B. The carrier mutations further implicated genetic counselling, and testing family members, if needed.
*Conclusions: Our study suggests that genetic testing in transplant recipients when used as a screening tool to reclassify patients, has low yield. However, a target screening approach (e.g. early onset ESRD, family history of ESRD etc) in the appropriate clinical phenotype may have higher yield for the test. The value addition and clinical criteria determination of genetic testing remains unknown. Further studies regarding the impact on value, downstream costs-savings and therapeutic interventions are much needed.
To cite this abstract in AMA style:
Sanchez-Garcia J, Morris D, Darling E, Dantis-Tan M, Olson J, Gaid K, Raza A, Anand S. Personalized Medicine Using Next-Generation Sequence for Kidney Transplant Recipients [abstract]. Am J Transplant. 2022; 22 (suppl 3). https://atcmeetingabstracts.com/abstract/personalized-medicine-using-next-generation-sequence-for-kidney-transplant-recipients/. Accessed February 22, 2026.« Back to 2022 American Transplant Congress