Patterns of Emergency Department (ED) Utilization between Transplant and Non-Transplant Centers and Impact on Clinical Outcomes in Kidney Recipients
MUSC, Charleston, SC
Meeting: 2019 American Transplant Congress
Abstract number: D178
Keywords: Graft failure, Kidney transplantation, Survival
Session Information
Session Name: Poster Session D: Non-Organ Specific: Disparities to Outcome and Access to Healthcare
Session Type: Poster Session
Date: Tuesday, June 4, 2019
Session Time: 6:00pm-7:00pm
 Presentation Time: 6:00pm-7:00pm
Presentation Time: 6:00pm-7:00pm
Location: Hall C & D
*Purpose: There is a high rate of ED utilization in kidney recipients post-transplant (txp); ED visits are associated with readmission rates and lower 3-yr survival rates. However, types of ED visits and utilization within and outside txp centers may lead to different outcomes. The objective of this study was to analyze ED utilization patterns at txp and non-txp centers and the impact on clinical outcomes. We sought to identify common etiologies of ED visits and their correlation with hospitalization and graft and patient outcomes.
*Methods: This was a longitudinal, retrospective, single center cohort study in kidney txp recipients evaluating ED utilization between 2007-2016. Data was obtained from the South Carolina All-Payer Public Use data files, which provides comprehensive utilization regardless of insurance. Comparator groups were determined by ED location, time from txp, and disposition/readmission from ED visit. Standard univariate statistics and multivariable Cox regression were utilized.
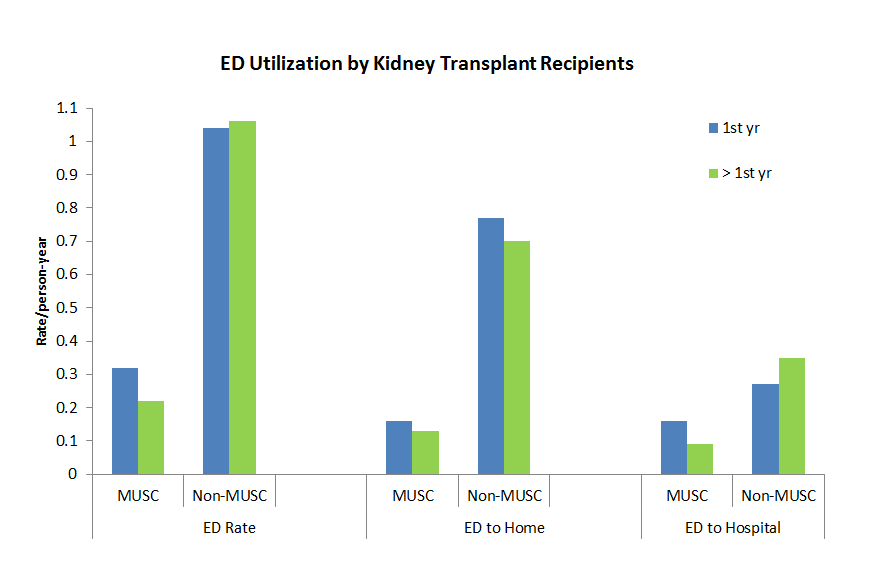
*Results: 1,106 kidney recipients were included, the majority were black, age >40 yrs, and recipients of a deceased donor (Table 1).Txp center ED utilization was 0.32, compared to 1.04 visits per patient-yr (VPPY) at a non-txp center during the first year post-txp (Figure 1). ED utilization dropped at the txp center after the 1st yr (p<0.001), while remaining similar at non-txp centers (0.22 vs 1.06 VPPY, respectively). Etiologic analysis revealed allograft complications was the most common cause of ED visits within the first yr, with infection being the most common >1 yr post-txp. In multivariable Cox modeling, the strongest risk factor for graft loss and death was an ED visit due to allograft complication at a non-txp center >1 yr post-txp (aHR 2.93 and aHR 1.75 respectively, p<0.0001) (Table 2).
*Conclusions: ED utilization significantly differs based on txp vintage; recent recipients tend to use the txp center ED more often, which decreases after >1 yr post-txp. Visits to non-txp center EDs for allograft dysfunction after >1 yr post-txp is the strongest predictor of subsequent graft loss and death, perhaps demonstrating that non-txp center EDs should not routinely manage txp-specific complications.
To cite this abstract in AMA style:
Perkins H, Patel N, Rohan V, Su Z, DuBay D, McGillicuddy J, Taber D. Patterns of Emergency Department (ED) Utilization between Transplant and Non-Transplant Centers and Impact on Clinical Outcomes in Kidney Recipients [abstract]. Am J Transplant. 2019; 19 (suppl 3). https://atcmeetingabstracts.com/abstract/patterns-of-emergency-department-ed-utilization-between-transplant-and-non-transplant-centers-and-impact-on-clinical-outcomes-in-kidney-recipients/. Accessed February 23, 2026.« Back to 2019 American Transplant Congress