Patient Response to a Formal Living Donor Liver Transplant Educational Program
Transplantation Center, Yale-New Haven Hospital, New Haven, CT
Meeting: 2019 American Transplant Congress
Abstract number: B331
Keywords: Donation, Ethics, Liver transplantation, Waiting lists
Session Information
Session Name: Poster Session B: Liver: Living Donors and Partial Grafts
Session Type: Poster Session
Date: Sunday, June 2, 2019
Session Time: 6:00pm-7:00pm
 Presentation Time: 6:00pm-7:00pm
Presentation Time: 6:00pm-7:00pm
Location: Hall C & D
*Purpose: Informed consent for liver waitlist candidates is required and includes discussion of donor graft options. Living donor liver transplant (LDLT) is an established option that addresses organ shortage, waitlist time, and offers excellent long term outcomes. Eligible patients may not be equipped with knowledge and resources to seek out this opportunity. We instituted a pilot education program on LDLT. We implemented a standardized workflow and aimed to assess patient response to the program.
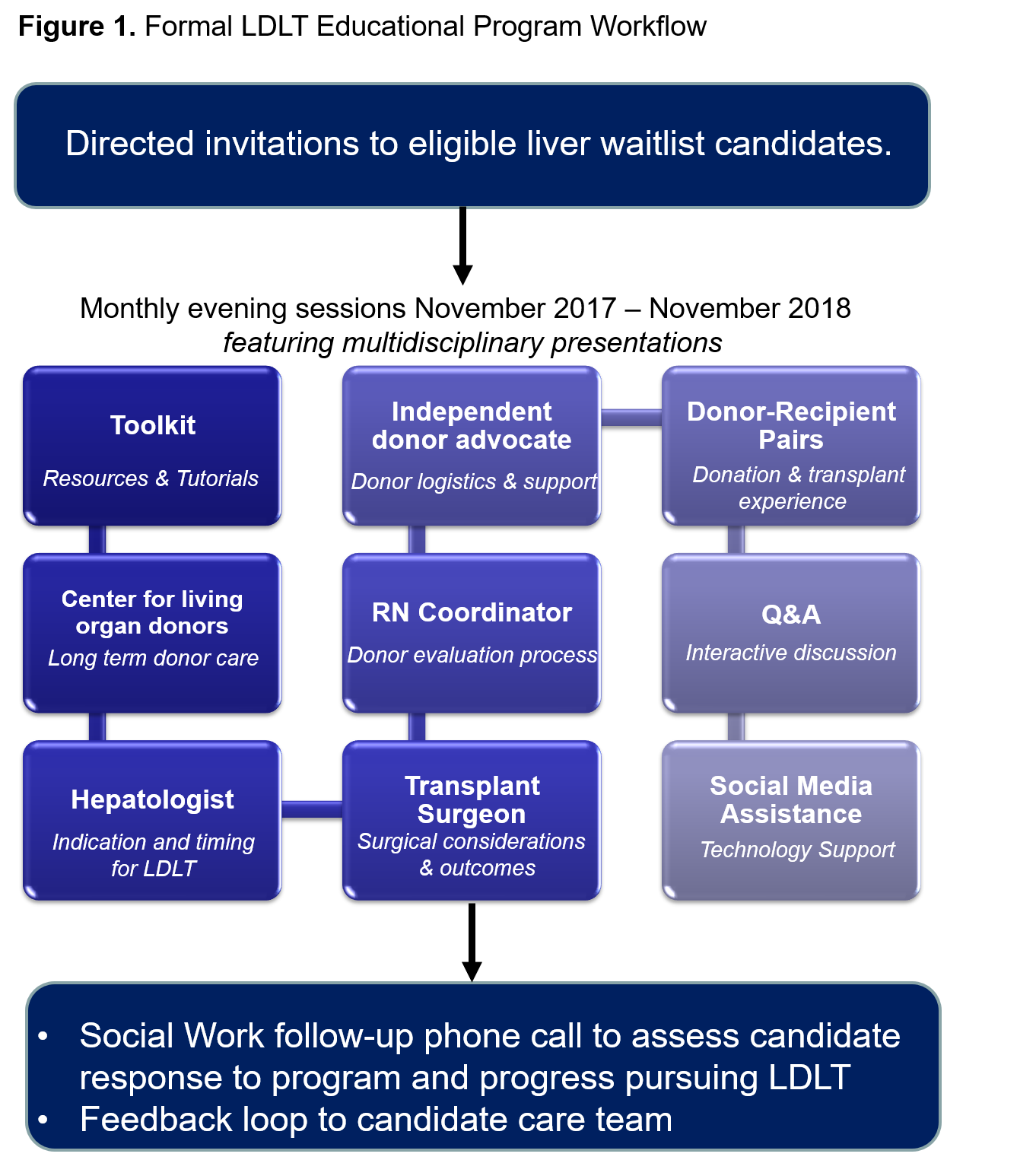
*Methods: Program workflow as in Figure 1. Participating candidates received a standardized follow-up phone call by their social worker. They were asked if they felt LDLT was an option for them, to rate the program, and to freely respond about the experience and steps they have taken to pursue LDLT. Demographic and descriptive data were analyzed.
*Results: Approximately 41% of the waitlist attended the program. The cohort was predominantly male (58%), Caucasian (88%) with an average age of 52 years. 74% (32/43) of participants were surveyed in a post-attendance call by their social worker. 97% (31/32) responded “Yes” they felt LDLT was an option for them. 12 participants provided a numerical program rating (avg 9.4 out of 10). 56% (24/43) participants have had donor referrals (range 1 to 91 referrals per patient, avg 10.4, SD18.1), 4 have approved living donors and 8 have been transplanted (2 LDLT, 6 DDLT). 20 participants specifically commented having taken action to pursue LDLT. Facebook was the most popular forum for candidates to share their story. The donor/recipient stories were noted to be a program strength. Representative participant quote: “I absolutely loved the program! I thought I knew enough, I did not. All patients should attend. So glad I attended. Willing to be a speaker if successfully transplanted with a living donor.” Not all program feedback was positive with some acknowledging feeling overwhelmed or ambivalent towards LDLT.
*Conclusions: A formal education program is well received by waitlist candidates and results in increased belief of LDLT as a viable and even favorable option. Participants free responses were useful in identifying common themes, program strengths, and areas for improvement. A standardized programmatic approach to raise awareness, and provide informed consent on LDLT is ethical, creates equal opportunity, and should be provided by transplant centers. Study expansion, ongoing data collection, and assessment of participant knowledge, will optimize the program and define its impact.
To cite this abstract in AMA style:
Narayanan P, Palumbo C, Ventura K, Tomlin R, Hammers L, Joyce M, Wuerth D, Haakinson D, Kulkarni S, Mulligan D, Emre S, Liapakis A. Patient Response to a Formal Living Donor Liver Transplant Educational Program [abstract]. Am J Transplant. 2019; 19 (suppl 3). https://atcmeetingabstracts.com/abstract/patient-response-to-a-formal-living-donor-liver-transplant-educational-program/. Accessed February 15, 2026.« Back to 2019 American Transplant Congress