Outcomes of Second Kidney Transplant After Return to Dialysis by Induction Type in the United States
1Medicine, University of Minnesota, Minneapolis, MN, 2Complex Care Analytics, M-Health Fairview, Minneapolis, MN, 3Surgery, University of Minnesota, Minneapolis, MN
Meeting: 2021 American Transplant Congress
Abstract number: 925
Keywords: Induction therapy, Outcome, Retransplantation
Topic: Clinical Science » Kidney » Kidney Immunosuppression: Induction Therapy
Session Information
Session Name: Kidney Immunosuppression: Induction Therapy
Session Type: Poster Abstract
Session Date & Time: None. Available on demand.
Location: Virtual
*Purpose: A failed kidney allograft is the 4th leading indication for kidney transplantation. We examined the association of induction use in 2nd kidney transplant recipients after returning to dialysis and the long-term recipient survival (RS) and death censored graft survival (DCGS).
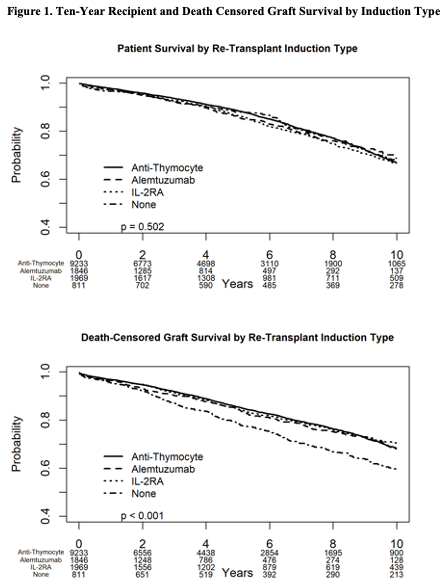
*Methods: Using the SRTR database, we identified all 2nd kidney recipients who returned to dialysis before re-transplantation. We excluded those with missing or unusual induction regimens, recipients with maintenance other than Tac and MMF +/- steroids and those with crossmatch positive results. We grouped recipients by induction type into 4 groups: Anti-thymocyte globulin (n=9233), Alemtuzumab (n=1846), IL-2RA (n=1969) and No-induction (n=811). We generated Kaplan-Meier curves of (RS) and (DCGS) with follow up censored at 10-year post-transplant. We used Cox proportional hazard (PH) models to examine the association of induction with these outcomes. We included center as a random effect. We adjusted for recipient age, gender, race, DM, PVD, ESRD etiology, donor type and gender, HLA-MM, steroid maintenance, time between transplants, payor type and transplant year. The (RS) model was stratified by transplant year; the (DCGS) model was stratified by time between transplants, time on dialysis, recipient age and donor age due to (PH) violations.
*Results: Rejection and PTLD rates at 1-year were not statistically different. DGF and re-hospitalization rates were lower, but mean creatinine was higher in the no induction group compared to the other groups. In the univariate analyses, (RS) did not differ by induction type (log-rank p=0.50). However, (DCGS) was the lowest in the no-induction group (log-rank p <0.001) (Figure 1). After adjustment, induction type was not a predictor of (RS) or (DCGS). Steroid maintenance was associated with better (DCGS) [aHR 0.86, 95% C.I. (0.76, 0.98), p=0.02]. Live-donor kidney was a favorable predictor of (RS) [aHR 0.75, 95% C.I. (0.67, 0.85), p<0.001] and (DCGS) [aHR 0.75, 95% C.I. (0.67, 0.85), p<0.001]. Publicly insured recipients had worse (RS) and (DCGS).
*Conclusions: In this large cohort of crossmatch negative second kidney transplant recipients, who were on dialysis prior to re-transplantation and discharged on Tac and MMF maintenance, recipients of no-induction had worse graft survival in the univariate analysis. In the fully adjusted models, induction type was not a predictor of (RS) or (DCGS). Live-donor kidneys improved recipient and graft survival.
To cite this abstract in AMA style:
Riad S, Shaker T, Jackson S, Kandaswamy R. Outcomes of Second Kidney Transplant After Return to Dialysis by Induction Type in the United States [abstract]. Am J Transplant. 2021; 21 (suppl 3). https://atcmeetingabstracts.com/abstract/outcomes-of-second-kidney-transplant-after-return-to-dialysis-by-induction-type-in-the-united-states/. Accessed February 17, 2026.« Back to 2021 American Transplant Congress