Organ Transplantation Associated with High Incidence of Anal Cancer and Pre-Cancer Lesions among HIV-Infected Women and Men
1University of California, San Francisco, San Francisco
2EMMES, Rockville
3Columbia University, New York
4University of Maryland, Baltimore
5Icahn School of Medicine at Mount Sinai, New York
6Cedars-Sinai Medical Center, Los Angeles
7Beth Israel Deaconess Medical Center, Boston.
Meeting: 2018 American Transplant Congress
Abstract number: 269
Keywords: HIV virus, Infection, Malignancy, Post-transplant malignancy
Session Information
Session Name: Concurrent Session: PTLD/Malignancies: All Topics
Session Type: Concurrent Session
Date: Monday, June 4, 2018
Session Time: 2:30pm-4:00pm
 Presentation Time: 2:54pm-3:06pm
Presentation Time: 2:54pm-3:06pm
Location: Room 4C-4
Objective: HIV-infected women and men and transplant recipients are two populations at increased risk of HPV-associated anal cancer but there is little published data. We determined anal cancer incidence and high-grade anal cytologic abnormalities (HSIL), and assessed factors associated with HSIL following organ transplantation in HIV-infected patients.
Methods: We followed 111 HIV-infected women and men who underwent liver (66%) and kidney (34%) transplantation at 6 academic centers in the U.S. During baseline (pre-transplantation) and follow-up visits post transplantation, we obtained anal cytology, demographics, and measured CD4+ T cells and HIV-1 plasma RNA.
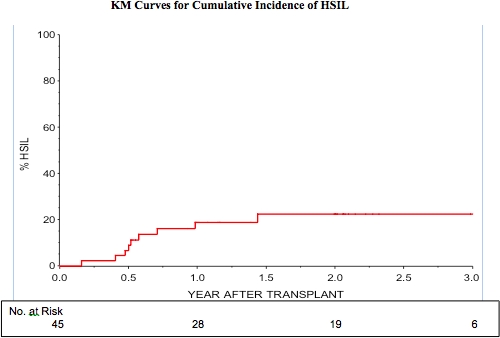
Results: At the baseline visit prior to receiving organ transplantation, 87% were male, 50% were men who had sex with men (MSM), median age was 49 (IQR 43-54), median CD4+ T cells was 371 (IQR, 252-571), and median HIV-1 plasma RNA was <50 copies/ml. Following transplantation, the incidence of anal cancer was 170 per 100,000 person-years. Of those with no disease at baseline, 9%, 19% and 22% were found to have HSIL at 6, 12 and 24 months post transplantation. In multivariable analyses, there was evidence for the association of nadir CD4 at enrollment (HR 1.3, 95% CI 1.03-1.6) and MSM behavior (HR 7.9, 95% CI, 1.0-64) with incident HSIL.
Conclusions: There is a high incidence of anal cancer and AIN among HIV-infected patients following transplantation. This is especially true since anal cytology underestimates the occurrence of AIN. Further studies will determine the optimal periodicity and timing of anal cancer screening among transplant recipients.
CITATION INFORMATION: Chin-Hong P., Barin B., Berry M., DaCosta M., Darragh T., Rosenthal L., Bartlett S., Dieterich D., Poordad F., Nissen N., Wong M., Stock P., Palefsky J. Organ Transplantation Associated with High Incidence of Anal Cancer and Pre-Cancer Lesions among HIV-Infected Women and Men Am J Transplant. 2017;17 (suppl 3).
To cite this abstract in AMA style:
Chin-Hong P, Barin B, Berry M, DaCosta M, Darragh T, Rosenthal L, Bartlett S, Dieterich D, Poordad F, Nissen N, Wong M, Stock P, Palefsky J. Organ Transplantation Associated with High Incidence of Anal Cancer and Pre-Cancer Lesions among HIV-Infected Women and Men [abstract]. https://atcmeetingabstracts.com/abstract/organ-transplantation-associated-with-high-incidence-of-anal-cancer-and-pre-cancer-lesions-among-hiv-infected-women-and-men/. Accessed March 6, 2026.« Back to 2018 American Transplant Congress