No Plan is a Bad Plan! Results of the American Society of Transplantation (AST) Living Donor Community of Practice Mortality Workgroup Survey on Disaster Planning Following a Living Donor Death
1Johns Hopkins, Baltimore, MD, 2Saint Louis University, St Louis, MO, 3University of Wisconsin, Madison, WI, 4University of Tennessee, Memphis, TN, 5Georgetown University, Washington, DC
Meeting: 2019 American Transplant Congress
Abstract number: B127
Session Information
Session Name: Poster Session B: Kidney Donor Selection / Management Issues
Session Type: Poster Session
Date: Sunday, June 2, 2019
Session Time: 6:00pm-7:00pm
 Presentation Time: 6:00pm-7:00pm
Presentation Time: 6:00pm-7:00pm
Location: Hall C & D
*Purpose: The risk of perioperative mortality following living kidney and liver donation, although extremely low, must not be considered a ‘never event’. While the risks of serious morbidity and mortality are minimized by thorough, multi-disciplinary evaluation, careful operative technique and postoperative care, anticipation of an untoward outcome is often a source of significant programmatic anxiety yet denial.
*Methods: A national survey of U.S. transplant surgeons was conducted to understand transplant programs’ experiences with and preparedness for the event of a living donor death. We distributed a 37-item, web-based survey to members of the American Society of Transplantation (AST) membership and community database.
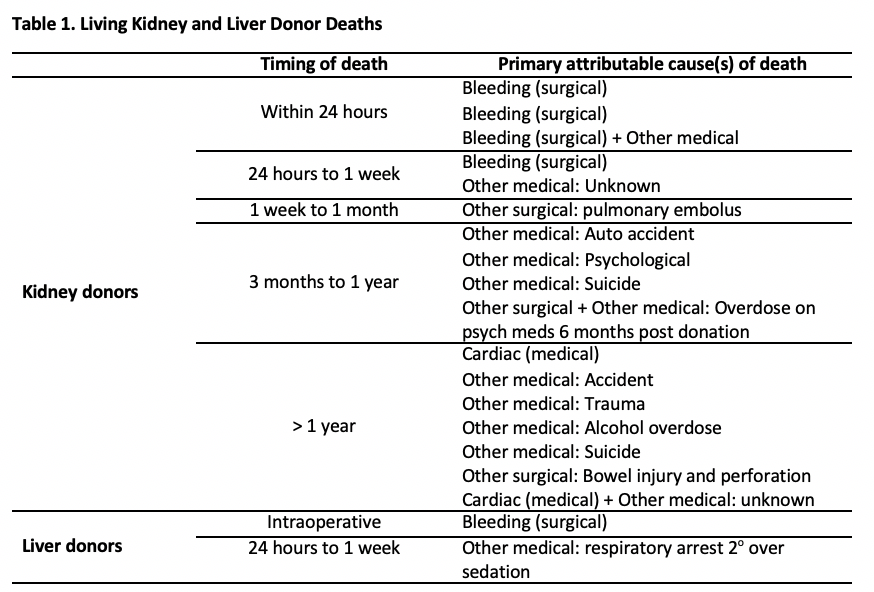
*Results: Respondents represented 87 unique transplant programs (71 kidney and 16 liver donor programs). Most respondents (N=68) reported no liver or kidney donor deaths within 2 years of donation at their program. Among 19 respondents who reported at least 1 kidney donor death, most (N=17) reported a single event. Living kidney donor deaths were attributed to surgical complications (N=6), suicide or psychological issues (N=5), accidents/trauma unrelated to donation (N=3), and medical or surgical complications unrelated to donation (N=2). Cause of death was not reported for 3 donors. Two respondents reported a single liver donor death at their respective transplant programs, both attributed to immediate surgical complications.
Although most respondents (N=57, 64% of total respondents; 88% of liver programs) reported being moderately to extremely concerned about a future living donor death at their institution, only 30 (33% of total program respondents) had a written plan available in the case of such an event. However, 63% of programs would find guidance and recommendations useful.
*Conclusions: While transplant clinicians struggle with the fear of a perioperative living donor death, most do not have prepared contingency plans. To help address this gap, the AST Living Donor COP will develop and present guidance for Disaster Planning suitable for implementation at US transplant programs including event analysis, team approach and roles, and communication strategies.
To cite this abstract in AMA style:
Henderson ML, Waldram MM, Lentine KL, Mandelbrot DA, Hays RL, Maluf DG, Cooper M. No Plan is a Bad Plan! Results of the American Society of Transplantation (AST) Living Donor Community of Practice Mortality Workgroup Survey on Disaster Planning Following a Living Donor Death [abstract]. Am J Transplant. 2019; 19 (suppl 3). https://atcmeetingabstracts.com/abstract/no-plan-is-a-bad-plan-results-of-the-american-society-of-transplantation-ast-living-donor-community-of-practice-mortality-workgroup-survey-on-disaster-planning-following-a-living-donor-death/. Accessed February 9, 2026.« Back to 2019 American Transplant Congress