Neutrophil to Lymphocyte Ratio (NLR) Does Not Predict Outcomes after Liver Transplant (LT) for Hepatocellular Carcinoma (HCC)
Hepatology, UCSF, San Francisco.
Meeting: 2018 American Transplant Congress
Abstract number: B266
Keywords: Inflammation, Risk factors, Survival, Tumor recurrence
Session Information
Session Name: Poster Session B: Liver: Hepatocellular Carcinoma and Other Malignancies
Session Type: Poster Session
Date: Sunday, June 3, 2018
Session Time: 6:00pm-7:00pm
 Presentation Time: 6:00pm-7:00pm
Presentation Time: 6:00pm-7:00pm
Location: Hall 4EF
Background: A high preoperative NLR ≥5 has been reported to predict poor outcomes following LT for HCC, and NLR has been incorporated into several prognostic models. The aim of this study was to assess the prognostic significance of NLR and changes in NLR over time prior to LT in a large cohort of HCC patients from a long wait time region. Methods: We evaluated 429 HCC patients who underwent LT with MELD exception from 2002-2015 at a single LT center. NLR was collected in all patients at LT and, if available, between 15-90 days prior to LT (NLR2; n=192). Patients were excluded from analysis because of peri-operative local-regional therapy (LRT, n=1) and culture-positive sepsis (n=2). Results: Median wait time from listing to LT was 11.1 months and 87% received LRT. Median NLR and NLR2 were 2.56 and 2.51, respectively. The median alpha-fetoprotein (AFP) at LT was 7.5 ng/mL. Patients with NLR ≥5 (n=64; 14.9%) exhibited no differences in tumor burden at LT listing, number of LRT, or AFP compared to patients with NLR <5. On explant, NLR ≥5 was associated with microvascular invasion (MVI) (p=0.037), tumor stage outside Milan criteria (p=0.035) and worse histologic grade (p=0.002). However, after a median post-LT follow-up of 4.7 years, the Kaplan-Meier survival and HCC recurrence rates were similar for NLR ≥5 vs NLR <5 (Figure) as was the time to HCC recurrence (p=0.60) and time to death (p=0.76). NLR2 was not predictive of post-LT survival or HCC recurrence, explant tumor stage, histologic grade, or MVI. The mean difference between NLR2 and NLR was 1.5 (range 0-20.8) and 47% of patients whose NLR2 was elevated ≥5 had an NLR <5 at LT. The direction and magnitude of the change in NLR did not correlate with post-LT recurrence or survival. 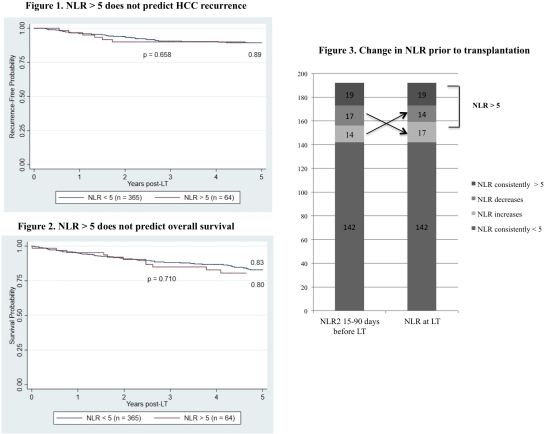 Conclusions: While NLR at LT correlated with MVI and tumor stage in explant, NLR did not predict post-LT survival or HCC recurrence. Further, NLR appeared to be a relatively unstable inflammatory marker with nearly half of all patients with NLR2 elevation potentially being incorrectly categorized as high-risk. These results did not support the use of NLR for HCC recurrence risk stratification or candidate selection for LT.
Conclusions: While NLR at LT correlated with MVI and tumor stage in explant, NLR did not predict post-LT survival or HCC recurrence. Further, NLR appeared to be a relatively unstable inflammatory marker with nearly half of all patients with NLR2 elevation potentially being incorrectly categorized as high-risk. These results did not support the use of NLR for HCC recurrence risk stratification or candidate selection for LT.
CITATION INFORMATION: Harding-Theobald E., Mehta N., Yao F. Neutrophil to Lymphocyte Ratio (NLR) Does Not Predict Outcomes after Liver Transplant (LT) for Hepatocellular Carcinoma (HCC) Am J Transplant. 2017;17 (suppl 3).
To cite this abstract in AMA style:
Harding-Theobald E, Mehta N, Yao F. Neutrophil to Lymphocyte Ratio (NLR) Does Not Predict Outcomes after Liver Transplant (LT) for Hepatocellular Carcinoma (HCC) [abstract]. https://atcmeetingabstracts.com/abstract/neutrophil-to-lymphocyte-ratio-nlr-does-not-predict-outcomes-after-liver-transplant-lt-for-hepatocellular-carcinoma-hcc/. Accessed February 20, 2026.« Back to 2018 American Transplant Congress
