National Landscape of Hope Act Transplant Candidates and Recipients in the United States
1Research, United Network for Organ Sharing, Richmond, VA, 2United Network for Organ Sharing, Richmond, VA
Meeting: 2019 American Transplant Congress
Abstract number: 12
Keywords: Donation, HIV virus, Kidney transplantation, Liver transplantation
Session Information
Session Name: Concurrent Session: Kidney Deceased Donor Allocation I
Session Type: Concurrent Session
Date: Sunday, June 2, 2019
Session Time: 2:30pm-4:00pm
 Presentation Time: 2:30pm-2:42pm
Presentation Time: 2:30pm-2:42pm
Location: Ballroom B
*Purpose: The HIV Organ Policy Equity (HOPE) Act, enacted on 11/21/13, allows for the transplantation of organs from HIV+ donors into HIV+ recipients in the United States under clinical research protocols. The OPTN revised organ allocation policies on 11/21/15, and on 11/23/15, research criteria were published and the Final Rule was revised accordingly.
*Methods: The OPTN database was used to describe the number and characteristics of HOPE Act waiting list (WL) registrations and deceased donor transplants (TX). HIV+ registrations were those waiting on the kidney (KI)/liver (LI) WL as of 9/30/18 that indicated willingness to accept an HIV+ organ. Transplants between 1/1/16-7/31/18 from donors with a positive test results for any HIV test collected by the OPTN were considered HOPE TXs.
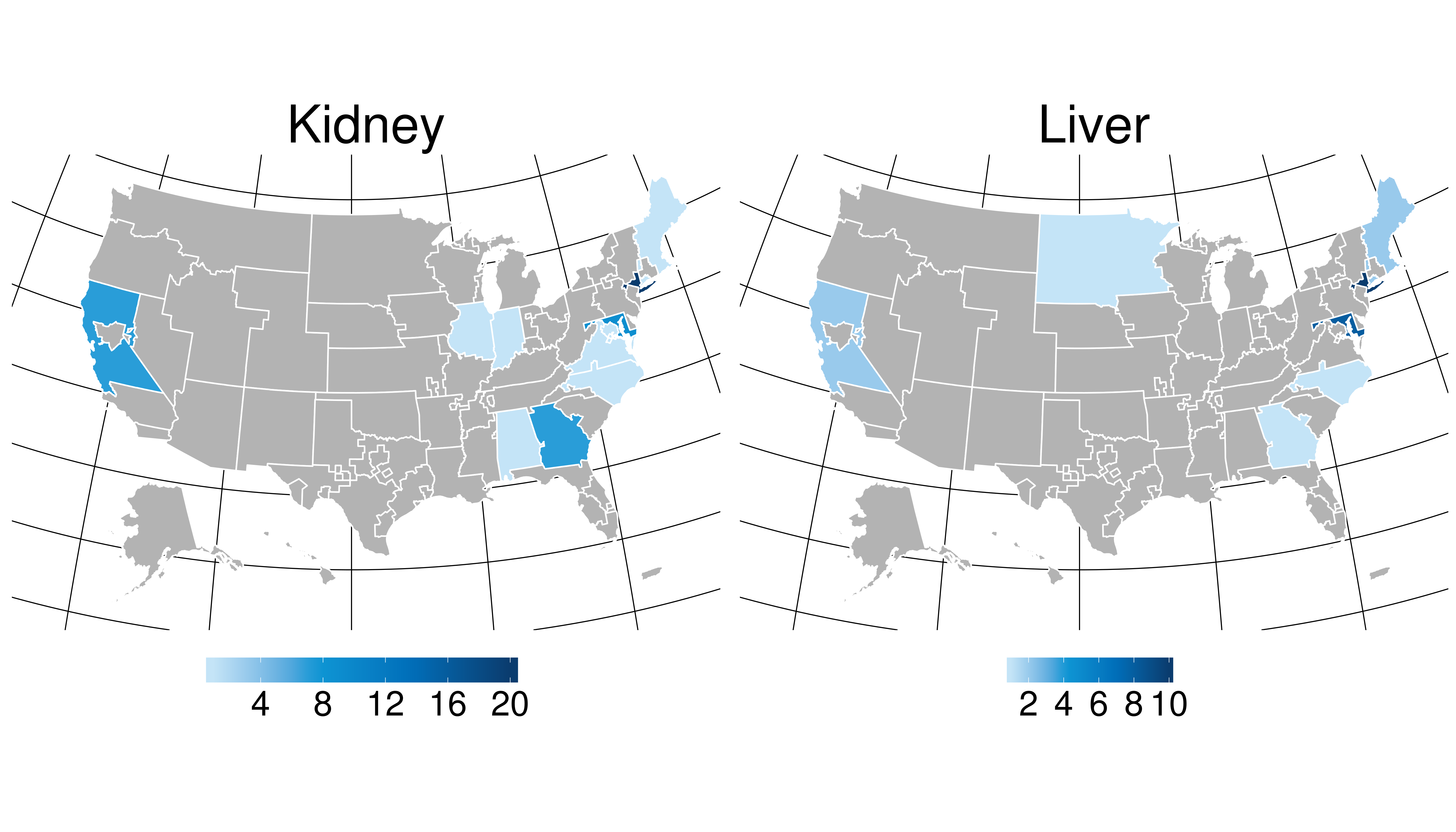
*Results: 218 registrations on the WL were indicated as willing to accept an HIV+ organ (199 KI, 19 LI). The mean organ acceptance rate across centers was higher for HIV+ KI and LI donors (35%, 69% respectively) than non-HIV+ (19%, 24% respectively). There have been 75 organs TXed (25 LI, 50 KI; 1 en bloc, 4 SLK). The number has varied quarterly with evidence of recent increases, with the majority occurring at few centers.
The majority of recipients were male (80%), White for KI (56%) but Black for LI (76%), blood type A or O (40%, 44% respectively), co-infected with HCV (33%) and/or HBV (76%), and occurred from organs outside of the transplanting hospital’s DSA (85%). Despite this, the median cold ischemic time (hours) remained similar to non-HIV+ (8 vs. 6 for LI, 18 vs. 16 for KI).
HIV+ KI recipients had a higher proportion of primary diagnosis for TX of HIV nephropathy and HCV, and HCV and HBV co-infection than non-HIV+ counterparts. HOPE Act TXs used lower KDPI kidneys in lower EPTS recipients who were less sensitized than HIV+ recipients of non-HIV+ KIs allocated through the usual allocation pathway. Specifically for HIV+ LI recipients, HOPE recipients were more likely to be TXed at lower MELD/PELD scores (median MELD at transplant 22 vs. 28) than other HIV+ recipients.
*Conclusions: Limited numbers of HOPE Act TX have been done to date. Recipients of HIV+ kidneys were younger, less sensitized, and received lower KDPI kidneys that non-HIV+ kidney recipients. The lower MELD score at TX for HOPE LI recipients compared to HIV+ non-HOPE and non-HIV+ LI recipients suggests that the HOPE Act may be increasing access to transplantation for this population. Increased utilization of the HOPE Act may provide additional TX opportunity for HIV+ recipients.
To cite this abstract in AMA style:
Wilk AR, Hunter R, McBride MA, Klassen DK. National Landscape of Hope Act Transplant Candidates and Recipients in the United States [abstract]. Am J Transplant. 2019; 19 (suppl 3). https://atcmeetingabstracts.com/abstract/national-landscape-of-hope-act-transplant-candidates-and-recipients-in-the-united-states/. Accessed February 19, 2026.« Back to 2019 American Transplant Congress