Mitigating the Adverse Impact of Broader Kidney Sharing with Hospital-based Machine Perfusion
Hackensack University Medical Center, Hackensack, NJ
Meeting: 2021 American Transplant Congress
Abstract number: 1259
Keywords: Allocation, Kidney, Preservation
Topic: Clinical Science » Organ Inclusive » Non-Organ Specific:Organ Preservation/Ischemia Reperfusion Injury
Session Information
Session Name: Non-Organ Specific: Organ Preservation/Ischemia Reperfusion Injury
Session Type: Poster Abstract
Session Date & Time: None. Available on demand.
Location: Virtual
*Purpose: The new UNOS kidney allocation changes effective December 2020 will be removing the geographic limits of donation service areas (DSA) and UNOS regions favoring a zone of 250 nautical miles (NM) from the donor hospital. Transplant centers with low waiting times will have access to fewer deceased donor kidneys (DDK) compared to transplant centers in neighboring DSAs with longer waiting times. This change will dramatically reduce locally allocated organs and broaden the sharing distance of lifesaving DDKs for our patients. In order to mitigate the risk of prolonged cold ischemic time (CIT) and to increase utilization of nationally shared kidneys, our center created a hospital-based machine preservation center utilizing hypothermic machine perfusion (HMP) in January of 2020. Implementation of HMP allowed improved evaluation of organs with higher KDPI and increased acceptance of kidneys with longer CIT. It is likely that organ procurement organizations might be less inclined to provide HMP with broader sharing of kidneys, making hospital access to HMP more vital. To our knowledge, only five centers in the US utilize hospital-based HMP.
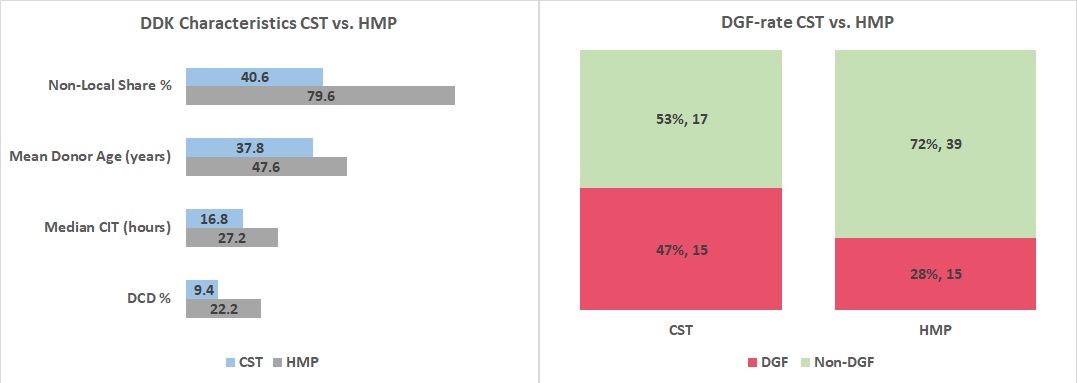
*Methods: A retrospective study compared characteristics and immediate outcomes of two groups of DDKs transplanted between January through October 2020: DDKs preserved with cold storage technique (CST) (N=32), and DDKs preserved using HMP (N=66). After organ evaluation on HMP, due to the higher machine-measured renal resistance and biopsy results, 12 (18.18%) kidneys were discarded and excluded from the study leaving this cohort with 54 kidneys.
*Results: Despite having a higher non-local share, a higher mean donor age, a higher median cold ischemic time (CIT), and a higher DCD rate), patients that received HMP kidneys have a significantly lower delayed graft function (DGF) and shorter median length of stay (LOS) compared to patients that received DDKs preserved with CST (p<0.01). No kidney in either cohort had primary non-function.
*Conclusions: HMP allowed us to get better access to non-local DDKs as it expanded our ability to evaluate nationally allocated kidneys that were locally declined, improved organ flush characteristics, alleviated risk of prolonged CIT while optimizing kidney function, and improved organ utilization. Other benefits included reduced hospital costs due to reduced LOS and DGF as well as transplanting patients faster and thus decreasing waitlist mortality and disease progression.
To cite this abstract in AMA style:
Yushkov Y, Schleich BR, Carrea T, Wadhera V, Goldstein MJ. Mitigating the Adverse Impact of Broader Kidney Sharing with Hospital-based Machine Perfusion [abstract]. Am J Transplant. 2021; 21 (suppl 3). https://atcmeetingabstracts.com/abstract/mitigating-the-adverse-impact-of-broader-kidney-sharing-with-hospital-based-machine-perfusion/. Accessed March 5, 2026.« Back to 2021 American Transplant Congress