Microvascular Inflammation without DSA or C4d: An Orphan Category in Banff Classification with Intense Capillaritis and Cytotoxic T-Cell Infiltration
1Nephrology Department, Hospital del Mar, Barcelona, Spain, 2Nephrology Department, IMIM - Institute Hospital del Mar for Medical Research, Barcelona, Spain, 3Pathology Department, Hospital del Mar, Barcelona, Spain
Meeting: 2020 American Transplant Congress
Abstract number: D-268
Keywords: Biopsy, Kidney transplantation
Session Information
Session Name: Poster Session D: Biomarkers, Immune Assessment and Clinical Outcomes
Session Type: Poster Session
Date: Saturday, May 30, 2020
Session Time: 3:15pm-4:00pm
 Presentation Time: 3:30pm-4:00pm
Presentation Time: 3:30pm-4:00pm
Location: Virtual
*Purpose: Antibody-mediated rejection (ABMR) associated with donor-specific HLA antibodies (DSA) is the leading cause of late allograft failure after kidney transplantation. Microvascular inflammation (MVI) without detectable circulating DSA or C4d + cannot be classified as ABMR according to Banff-2017. The involvement of intragraft lymphocyte subsets in the development of humoral damage in kidney transplantation (KT) is relevant. We aimed to analyze lymphocyte subset distribution in kidney transplant biopsies (KTBx) with ABMR compared with MVI and with normal KTBx.
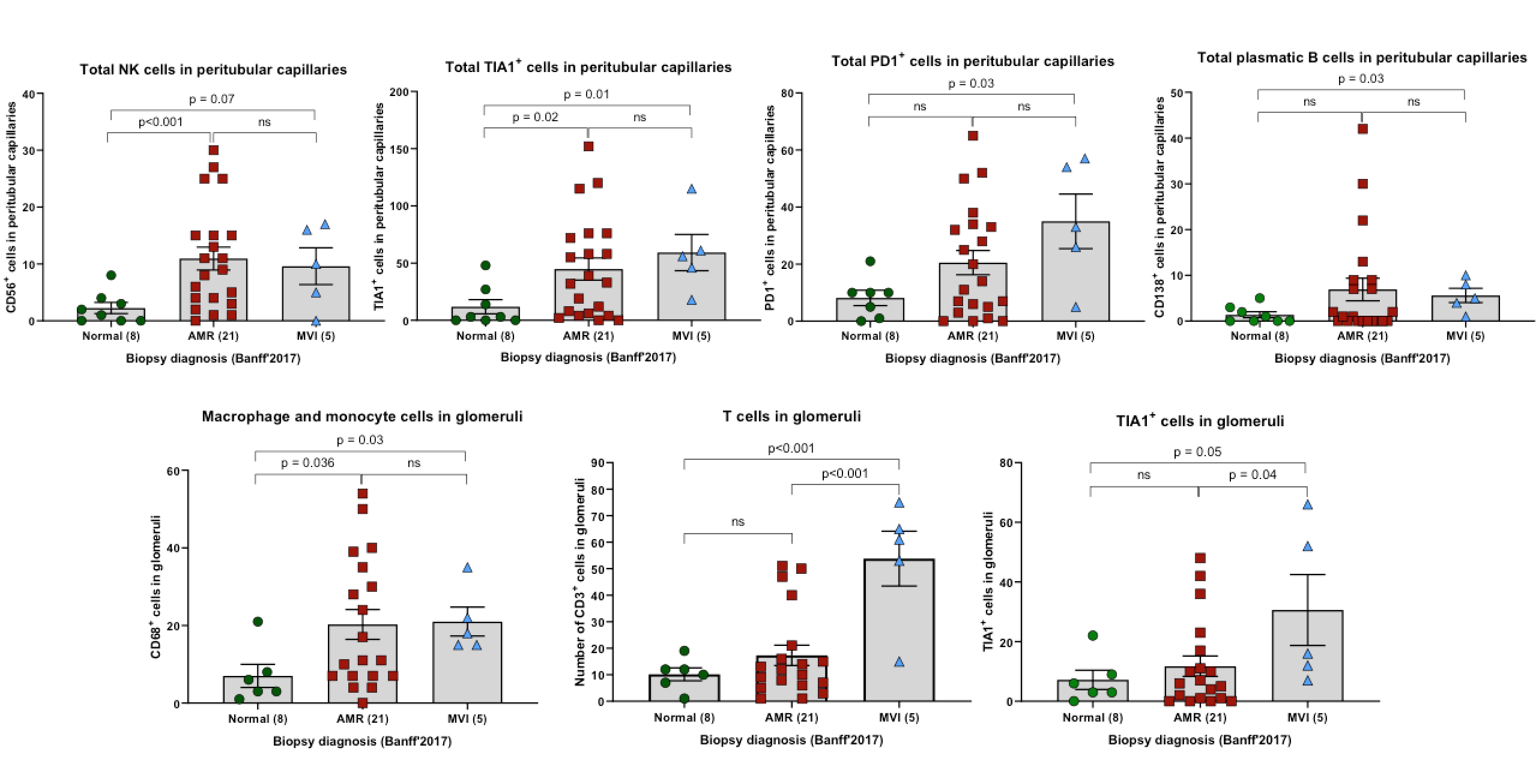
*Methods: KTBx with ABMR, MVI (g+ptc≥2, without DSA) or normal findings were included. DSA were identified with Luminex single antigen assays. Intragraft lymphocyte subsets’ characterization was performed by immunohistochemistry: T-lymphocytes (CD3, CD4, CD8, Foxp3), B-lymphocytes / plasmatic cells (CD20, CD138), NK cells (CD56), macrophages / monocytes (CD68), cytotoxic cells (TIA1) and activated cells (PD1) were evaluated.
*Results: We analyzed 34 KTBx: 21 ABMR, 5 MVI and 8 KTBx with normal findings. KT with ABMR and MVI had more proteinuria at the time of the biopsy compared with the normal group (575 mg/24h and 964 mg/24h vs 147 mg/24h, p=0.002 and p=0.005 respectively). DSA were more frequently detected in patients with ABMR (95.2% vs 0% and 37.5%, p<0.001 and p=0.003 respectively). KTBx with ABMR and MVI had increased cytotoxic T-cell infiltration apparently corresponding to NK cells in peritubular capillaries (ptc) compared to normal group. Moreover, both groups showed a greater number of macrophages and monocytes in glomeruli. KT with MVI but not with ABMR had a significantly increased activated cell infiltration (PD1+) in ptc compared to the normal group, and showed an increased cytotoxic T-cell infiltration in glomeruli compared to ABMR and normal groups.
*Conclusions: ABMR and MVI have an increased infiltration of NK cells with cytotoxic activity in ptc that differs from the normal group. However, KT with MVI show greater infiltration of activated cells in ptc and cytotoxic T-cell in glomeruli compared to ABMR suggesting the possibility of different activation pathways.
To cite this abstract in AMA style:
Buxeda A, Llinàs-Mallol L, Gimeno J, Arias-Cabrales C, Burballa C, Redondo-Pachón D, Raïch-Regué D, Pérez-Sáez M, Pascual J, Crespo M. Microvascular Inflammation without DSA or C4d: An Orphan Category in Banff Classification with Intense Capillaritis and Cytotoxic T-Cell Infiltration [abstract]. Am J Transplant. 2020; 20 (suppl 3). https://atcmeetingabstracts.com/abstract/microvascular-inflammation-without-dsa-or-c4d-an-orphan-category-in-banff-classification-with-intense-capillaritis-and-cytotoxic-t-cell-infiltration/. Accessed February 22, 2026.« Back to 2020 American Transplant Congress