Microvascular Inflammation in Early Protocol Biopsies of Renal Allografts in Cases of Chronic Active Antibody-Mediated Rejection
1Demartment of Pathology, Sapporo City General Hospital, Sapporo, Japan
2Department of Kidney Transplant Surgery, Sapporo City General Hospital, Sapporo, Japan.
Meeting: 2015 American Transplant Congress
Abstract number: 90
Keywords: Kidney transplantation, MHC class II, Microcirculation, Protocol biopsy
Session Information
Session Name: Concurrent Session: Kidney Antibody Mediated Rejection II
Session Type: Concurrent Session
Date: Sunday, May 3, 2015
Session Time: 4:00pm-5:30pm
 Presentation Time: 4:00pm-4:12pm
Presentation Time: 4:00pm-4:12pm
Location: Terrace I-III
Aim:
Chronic active antibody-mediated rejection (chronic ABMR) is one important cause of late-stage renal allograft loss. However, few reports have used protocol biopsy to observe changes over time in cases that develop chronic ABMR. The aim of this study was to use protocol biopsy to clarify the histological features of cases that develop chronic ABMR.
Methods:
We recruited 379 ABO compatible patients who underwent protocol biopsy at our hospital from 2010 to 2014. Seventeen of these patients were diagnosed with chronic ABMR (chronic ABMR group), and 12 patients were class 2 donor-specific antibody (DSA) positive and were not diagnosed with chronic ABMR (class 2 DSA-positive group). With the addition of a control group consisting of 30 DSA negative patients, these three groups were compared for Banff factors in protocol biopsies taken 3 months, 6 months, 1 year, 3 years, and 5 years after the transplant.
Results:
Three months post transplant, the chronic ABMR group had a significantly higher number of patients exhibiting g + ptc > 0 than that in the control group (p=0.01). At 1, 3, and 5 years post transplant, significantly more subjects in the chronic ABMR and class 2 DSA-positive groups compared with the control group exhibited g + ptc > 0 (p<0.03). Five years post transplant, the chronic ABMR group exhibited a significantly higher mean c4d score than that in the control group (p=0.02). The only significant difference observed between the chronic ABMR group and the class 2 DSA-positive group was in cg scores at 5 years post transplant, which were significantly higher in the chronic ABMR group (p=0.03).
Conclusions:
These results suggest that cases exhibiting microvascular inflammation in the early post-transplant period may develop chronic ABMR, and it would be highly beneficial to perform focused electron microscope surveillance of these cases. 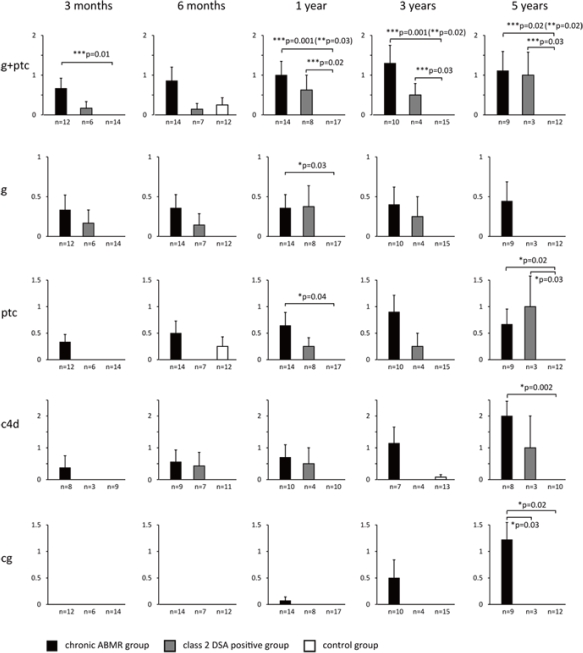
To cite this abstract in AMA style:
Tsuji T, Yanai M, Itami H, Ishii Y, Akimoto M, Fukuzawa N, Harada H, Fukasawa Y. Microvascular Inflammation in Early Protocol Biopsies of Renal Allografts in Cases of Chronic Active Antibody-Mediated Rejection [abstract]. Am J Transplant. 2015; 15 (suppl 3). https://atcmeetingabstracts.com/abstract/microvascular-inflammation-in-early-protocol-biopsies-of-renal-allografts-in-cases-of-chronic-active-antibody-mediated-rejection/. Accessed February 25, 2026.« Back to 2015 American Transplant Congress
