Microcirculation Inflammation with TCMR is Associated with Poor Graft Outcomes in Kidney Transplant Recipients (KTRs) without ABMR
UPMC, Pittsburgh, PA
Meeting: 2019 American Transplant Congress
Abstract number: C150
Keywords: Inflammation, Outcome
Session Information
Session Name: Poster Session C: Kidney: Acute Cellular Rejection
Session Type: Poster Session
Date: Monday, June 3, 2019
Session Time: 6:00pm-7:00pm
 Presentation Time: 6:00pm-7:00pm
Presentation Time: 6:00pm-7:00pm
Location: Hall C & D
*Purpose: Glomerulitis (g) and peritubular capillaritis (ptc), defined as microcirculation inflammation lesions (MI), are a hallmark of ABMR in KTRs. Their significance in KTRs with various grades of tubulo-interstitial inflammation is less known.
*Methods: In this prospective study, we analyzed the significance of MI,detected within the 1st post-transplant year using serial biopsies (for-cause & protocol-3 &12mo) and their association with varying grades of TCMR.
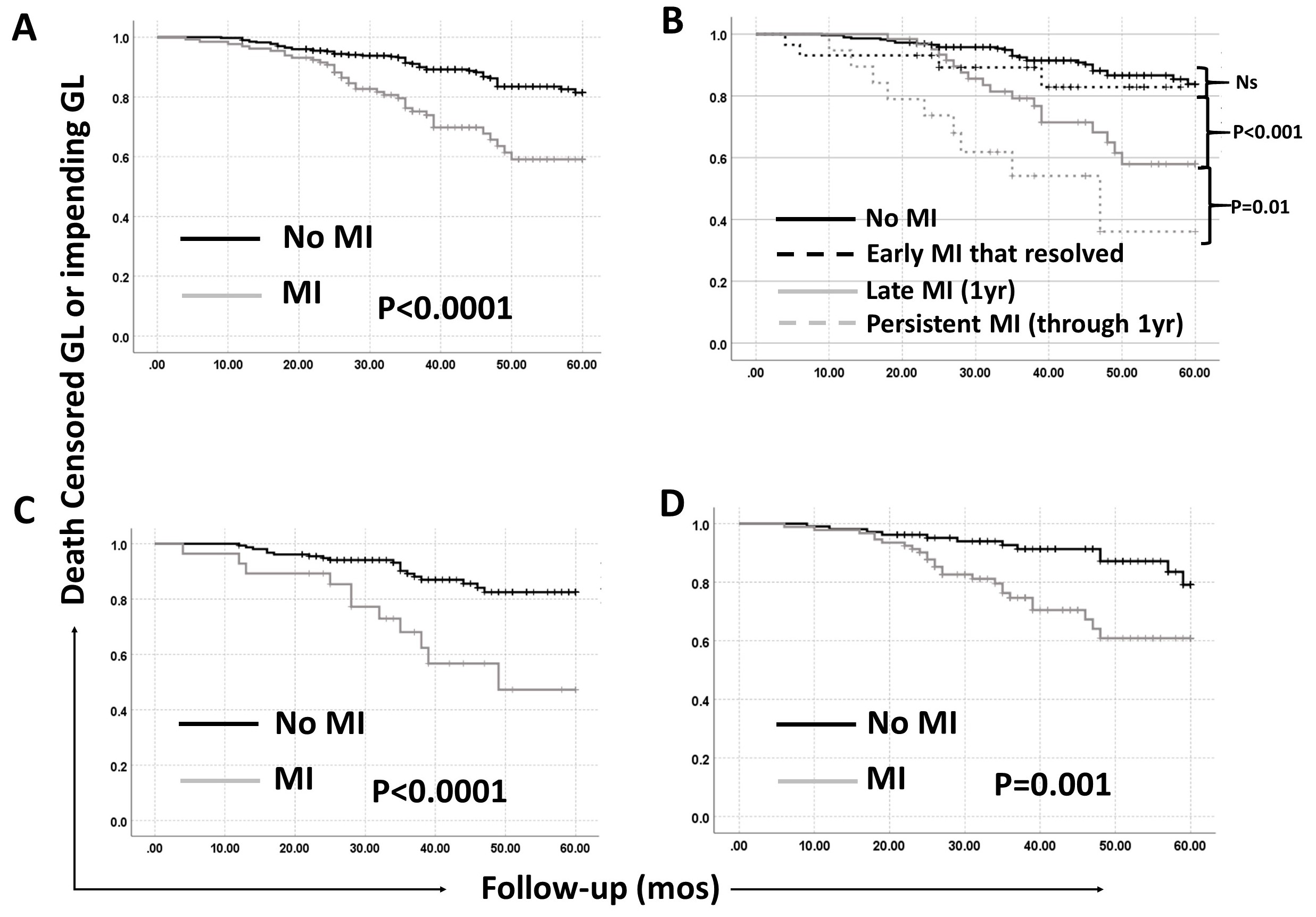
*Results: 594/755 KTRs (01-13 to 12-16) had serial biopsies along with DSA assessment (0,1,3,6,9&12mo) through the 1st post-transplant year. 24 KTRs with ABMR, and 26 with either GN/BKVN were excluded. Of the 544 remaining KTRs, 37% had TCMR (12% clinical (ACR) & 25% sub-clinical (SCR)) in the first post-transplant year. Of these 544 KTRs, 25% had either ‘g’ or ‘ptc’ lesions in the 1st year. Whilst 7% KTRs had ‘g’ lesions and 13% had ‘ptc’ lesions alone, 5% KTRs had both ‘g’ and ‘ptc’ lesions. Further, 7% of KTRs had ‘g+ptc’ score≥2. Analysis of serial biopsies showed that while 22% of KTRs had early MI that resolved; 60% had late MI at 1yr biopsy while 18% had persistent/recurrent MI through the 1st yr. 7% of patients with no TCMR, 15% with Borderline TCMR, 38% with sub-clinical and 64% with clinical TCMR had MI. While 61% of KTRs with Banff 1B TCMR had MI, even in those with Banff 1A TCMR, 41% had these lesions. Thus, MI was seen in both very early post-transplant period and at 1 yr and importantly was associated with even low grade TCMR as well. MI, especially in association with TCMR was associated with significantly worse IFTA (p<0.001) at1yr. MI was associated with significantly increased graft loss or impending graft loss (eGFR<30ml/min with>30% decline from baseline) (Fig 1A). Increasing severity of MI along with late or persistent MI at 1yr was associated with progressively worse graft outcome (Fig 1B). The combination of MI with TCMR was associated with the highest rate of graft loss or impending graft loss. Importantly, MI risk stratified both borderline (Fig 1C) and Banff 1A or greater TCMR (Fig 1D), being associated with worse outcome. Finally, in a multivariate Cox model, MI+TCMR is independently associated with worse graft outcome.Thus, patients with MI+TCMR represent a very high-risk group for poor graft outcomes.
*Conclusions: MI is associated with even milder grades of TCMR in the absence of ABMR or GN. Importantly, the presence of MI helps to risk stratify various grades of TCMR. Patients with TCMR should be examined closely for the presence of MI, as they represent a high-risk group who might benefit from enhanced IS with newer therapeutic agents.
To cite this abstract in AMA style:
Cherukuri A, Tandukar S, Hariharan S, Mehta R. Microcirculation Inflammation with TCMR is Associated with Poor Graft Outcomes in Kidney Transplant Recipients (KTRs) without ABMR [abstract]. Am J Transplant. 2019; 19 (suppl 3). https://atcmeetingabstracts.com/abstract/microcirculation-inflammation-with-tcmr-is-associated-with-poor-graft-outcomes-in-kidney-transplant-recipients-ktrs-without-abmr/. Accessed February 22, 2026.« Back to 2019 American Transplant Congress