Microcirculation Inflammation Is Superior to Peritubular Capillary Basement Membrane Multilayering for Outcome Prediction in Renal Transplant Patients with De Novo Donor-Specific Antibodies
Imperial College NHS Trust, London, United Kingdom
, United Kingdom
Meeting: 2013 American Transplant Congress
Abstract number: 31
In renal transplant patients with de novo donor-specific antibodies (DSA) we compared peritubular capillary basement membrane multilayering (PTCBML) counts with microcirculation inflammation (MI) score to predict development of transplant glomerulopathy (TG) and renal graft failure.
The first biopsy after transplantation with material available for electron microscopy was classified according to Banff '09 (n=52). De novo DSA were defined by negative donor-specific Luminex single antigen beads (MFI<300) before transplantation, and after transplantation DSA with a MFI>500. BML was scored in 25 PTC. PTCBML+ was defined as an average of ≥2 layers (n=22). MI, defined by the combination of glomerulitis (g) and peritubular capillaritis (ptc), was positive when MI score was ≥2 (n=17). Median follow-up from biopsy: 3.4 (IQR 2.0 to 4.7) years. Median time to biopsy: 0.7 (IQR 0.4 to 1.7) years. Median time between DSA development and biopsy: 0.3 (IQR -0.1 to 0.9) years. The Kaplan-Meier product limit method was used to estimate time to TG development and renal graft failure.
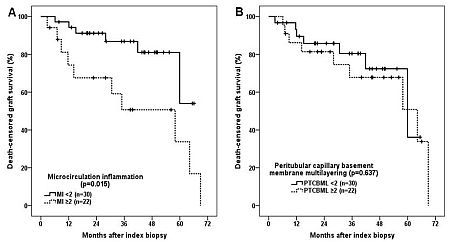
MI and PTCBML score did not correlate with each other (p=0.136). MI and PTCBML score were not significantly associated with time to biopsy from transplantation or with time from DSA development to biopsy. An MI+ score on index biopsy was associated with worse graft survival (Figure 1A) (p=0.015), while PTCBML count (Figure 1B) (p=0.637) did not correlate.
TG development could only be assessed in 42 patients as 10 patients had no follow-up biopsy (n=9) or had TG on index biopsy (n=1). MI+ and PTCBML+ score both associated with TG development (p=0.007 and p=0.020, respectively).
In renal transplant patients with de novo DSA, PTCBML count is inferior to MI score for prediction of graft survival. MI score and PTCBML count are both associated with TG development. In this population, PTCBML count does not add information to the MI score in the early post-transplant period to assess antibody-mediated injury to the graft.
To cite this abstract in AMA style:
Kort Hde, Willicombe M, Brookes P, Moran L, Santos-Nunez E, Galliford J, Taube D, McLean A, Moss J, Cook H, Roufosse C. Microcirculation Inflammation Is Superior to Peritubular Capillary Basement Membrane Multilayering for Outcome Prediction in Renal Transplant Patients with De Novo Donor-Specific Antibodies [abstract]. Am J Transplant. 2013; 13 (suppl 5). https://atcmeetingabstracts.com/abstract/microcirculation-inflammation-is-superior-to-peritubular-capillary-basement-membrane-multilayering-for-outcome-prediction-in-renal-transplant-patients-with-de-novo-donor-specific-antibodies/. Accessed July 15, 2025.« Back to 2013 American Transplant Congress
