Meta-Analysis of Clinical Significance of Complement Activating Anti-HLA DSA in Kidney Transplantation.
1Paris Translational Research Center for Organ Transplantation, Paris, France
2Department of Nephrology, Dialysis and Transplantation, Liège, Belgium
Meeting: 2017 American Transplant Congress
Abstract number: 297
Keywords: HLA antibodies, Kidney transplantation, Outcome, Rejection
Session Information
Session Name: Concurrent Session: Antibody Mediated Rejection in Kidney Transplant Recipients: Pathophsiology and Epidimiology
Session Type: Concurrent Session
Date: Monday, May 1, 2017
Session Time: 4:30pm-6:00pm
 Presentation Time: 4:42pm-4:54pm
Presentation Time: 4:42pm-4:54pm
Location: E354a
Donor-specific anti-HLA antibodies (DSA) are currently recognized as the major limitation to access transplantation and the first cause of late transplant failures. The effect of complement activating DSA on allograft rejection and graft loss has been diversely reported with varying amplitudes between studies.
We report the results of a systematic review and meta-analysis of complement activating DSA and their association with graft outcomes in renal transplant recipients. We searched on PubMed, Elsevier Science Direct and Cochrane databases using the following search terms “kidney transplantation, complement-activating DSA, IgG subclass, C1q, C4d, C3d, graft survival and antibody-mediated rejection”.
A total of 825 records published between 2004 and 2016 were identified by the search procedure. Duplicate records were removed. We also eliminated case-reports, reviews and studies including less than 10 patients. We included studies using single–antigen flow bead techniques. Studies focusing on non-DSA were excluded. The primary outcome was graft survival and the secondary outcome was antibody-mediated rejection rate. The search identified 34 cohort studies comprising a total of 7.293 kidney transplant patients. Studies with available data on primary and secondary outcomes were finally used in the complete meta-analysis, summing up 21 studies and 5.592 patients.
Together, these studies demonstrate that patients with post transplant circulating complement activating anti-HLA DSA defined by C1q, C4d, C3d binding capacity or IgG3 subclass show an increased risk of antibody-mediated rejection with a pooled HR of 8.40 (95%CI: 5.21–13.56) and an increase risk of graft loss with a pooled HR of 4.88 (95%CI: 4.03–5.91) and i2 of 58.5%. 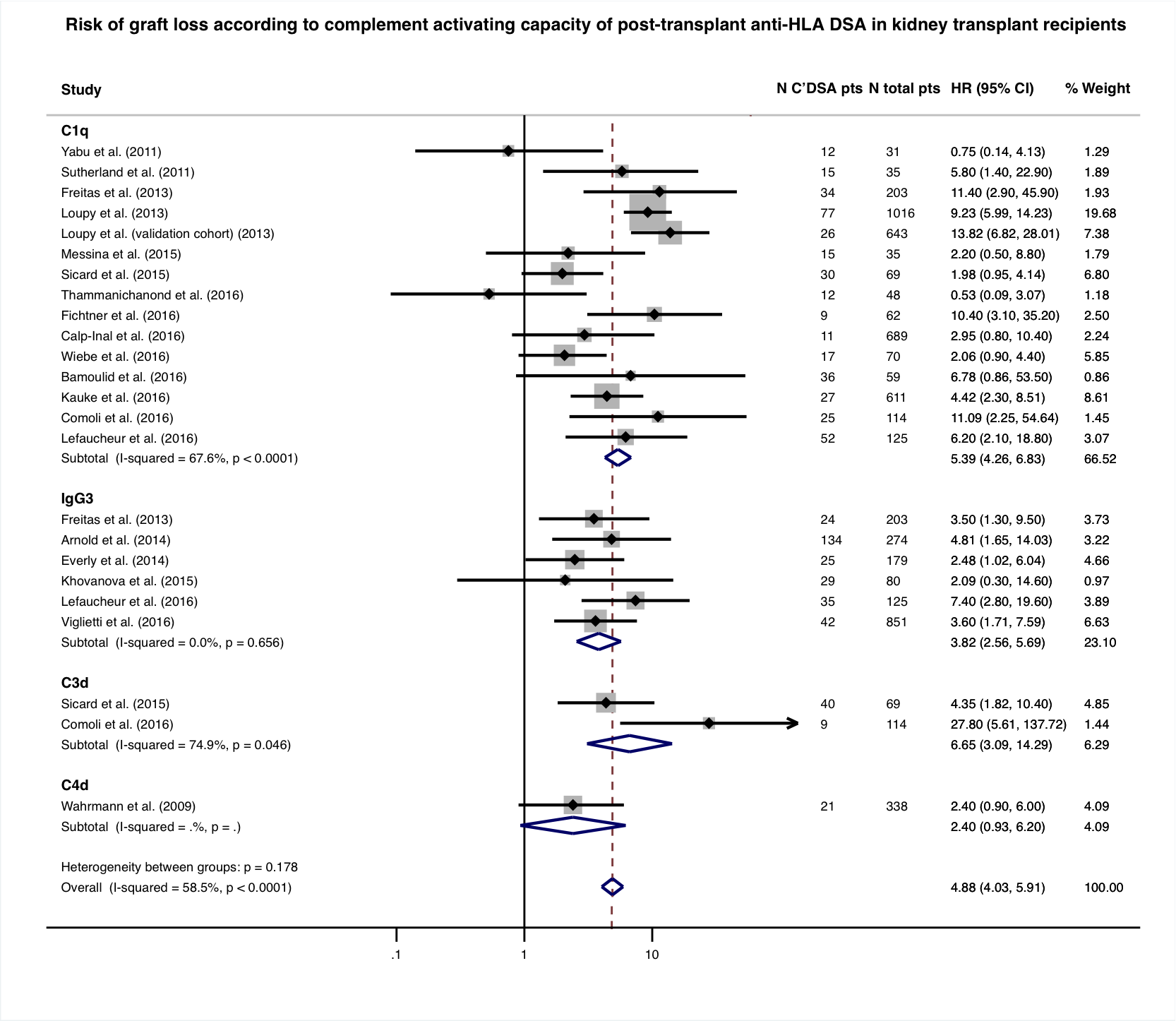 Complement activating DSA are strongly associated with increased risk of antibody-mediated graft rejection and impaired long term allograft survival. Future studies are needed to define the place of complement activating DSA in the clinical-decision making for kidney transplant recipients.
Complement activating DSA are strongly associated with increased risk of antibody-mediated graft rejection and impaired long term allograft survival. Future studies are needed to define the place of complement activating DSA in the clinical-decision making for kidney transplant recipients.
CITATION INFORMATION: Bouquegneau A, Ulloa C, Aubert O, Loheac C, Viglietti D, Empana J, Jabre P, Jouven X, Lefaucheur C, Loupy A. Meta-Analysis of Clinical Significance of Complement Activating Anti-HLA DSA in Kidney Transplantation. Am J Transplant. 2017;17 (suppl 3).
To cite this abstract in AMA style:
Bouquegneau A, Ulloa C, Aubert O, Loheac C, Viglietti D, Empana J, Jabre P, Jouven X, Lefaucheur C, Loupy A. Meta-Analysis of Clinical Significance of Complement Activating Anti-HLA DSA in Kidney Transplantation. [abstract]. Am J Transplant. 2017; 17 (suppl 3). https://atcmeetingabstracts.com/abstract/meta-analysis-of-clinical-significance-of-complement-activating-anti-hla-dsa-in-kidney-transplantation/. Accessed March 4, 2026.« Back to 2017 American Transplant Congress
