Membranoproliferative Glomerulonephritis After Kidney Transplantation: A Single Center Experience
The Johns Hopkins University, Baltimore, MD.
Meeting: 2015 American Transplant Congress
Abstract number: A55
Keywords: Glomerulonephritis, Recurrence, Risk factors
Session Information
Session Name: Poster Session A: Delayed Function/Acute Injury/Outcomes/Glomerulonephritis
Session Type: Poster Session
Date: Saturday, May 2, 2015
Session Time: 5:30pm-7:30pm
 Presentation Time: 5:30pm-7:30pm
Presentation Time: 5:30pm-7:30pm
Location: Exhibit Hall E
Introduction: Membranoproliferative glomerulonephritis (MPGN) is a glomerular disease that frequently leads to ESRD requiring dialysis or kidney transplantation. MPGN recurrence after transplant (rMPGN) often happens and may lead to allograft failure. Data on rMPGN course and its management is still limited. We present our single center data on rMPGN.
Patients & Methods: We identified 33 patients with ESRD due to different types of MPGN who received 39 total kidney transplantations in our institution between Jan 1994 and Sep 2013. Patients' characteristics are shown in table 1.
| Mean age at transplantation (yr) | 36.5 |
| Sex | 16M/17F |
| Race | 24/33 (69%) Caucasian, 5/33 (15%) African American, 4/33 (15%) other |
| MPGN type | Type I 65%, Type II 10%, Type III 25% |
| Donor source | Deceased 10, living unrelated 14, living related 15 |
| Preemptive/Non-preemptive | 4/35 |
| Cumulative ESRD duration (yr) | 5.4 |
Results: Mean time of follow-up was 4.6 years. rMPGN was detected in 16 out of the 39 transplants (41%). 8 of 11 (72%) patients who developed rMPGN and had complement levels available, had low C3 or C4 level. Whereas all (100%) 8 patients who had no recurrence and had complement levels available had normal C3 and C4 levels (p 0.002). Preemptive transplant was associated with increased risk of rMPGN (p 0.03). Gender, race, source of transplant, and age at transplant were not different between the two groups. In 10 out of the 16 (62%) transplants who developed rMPGN, the recurrence led to graft loss, whereas only 7 transplants out of the 23 (30%) without rMPGN developed graft loss (p 0.048). Treatment of rMPGN is shown in table 2.
| Therapy | Success Rate |
| Steroids | 1/4 |
| Rituximab +/- plasmapheresis | 2/6 |
| Plasmapheresis alone | 1/1 |
| Non-immunosuppressive | 3/5 |
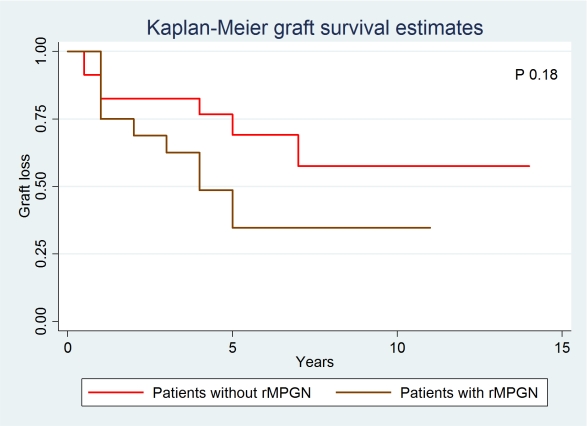
Conclusion: Our study suggests that the risk of rMPGN significantly increases with low complement level before or at time of transplantation and in cases of preemptive transplants. Our data also suggests that rMPGN after transplantation is associated with significant renal allograft loss and poor response to therapy.
To cite this abstract in AMA style:
Alasfar S, Carter-Monroe N, Rosenberg A, Montgomery R, Alachkar N. Membranoproliferative Glomerulonephritis After Kidney Transplantation: A Single Center Experience [abstract]. Am J Transplant. 2015; 15 (suppl 3). https://atcmeetingabstracts.com/abstract/membranoproliferative-glomerulonephritis-after-kidney-transplantation-a-single-center-experience/. Accessed February 28, 2026.« Back to 2015 American Transplant Congress
