Meld/Peld Exception Policy and Outcomes in Children with Hepatopulmonary Syndrome Requiring Liver Transplantation in the United States
1Keck School of Medicine of USC, Los Angeles, CA, 2Surgery, University of Southern California, Los Angeles, CA, 3University of Southern California, Los Angeles, CA, 4Liver Transplant Program, Children's Hospital-Los Angeles, Los Angeles, CA
Meeting: 2022 American Transplant Congress
Abstract number: 331
Keywords: Allocation, Hepatopulmonary syndrome, Liver transplantation, Pediatric
Topic: Clinical Science » Liver » 61 - Liver: Pediatrics
Session Information
Session Time: 5:30pm-7:00pm
 Presentation Time: 6:40pm-6:50pm
Presentation Time: 6:40pm-6:50pm
Location: Hynes Room 311
*Purpose: Hepatopulmonary syndrome (HPS) is associated with increased waitlist mortality in liver transplant (LT) candidates. Children with HPS are currently granted MELD/PELD exception for LT prioritization in the U.S. based on criterion developed for adults. The purpose of this study was to assess the impact of this MELD/PELD exception policy on children with HPS.
*Methods: A retrospective cohort of patients <18 years with a MELD/PELD exception request for HPS between 2007-2018 were identified in the SRTR. Patient characteristics and HPS criteria from exception narratives were examined. Patients were stratified by waitlist PaO2 to assess risk factors for waitlist mortality and post-LT survival.
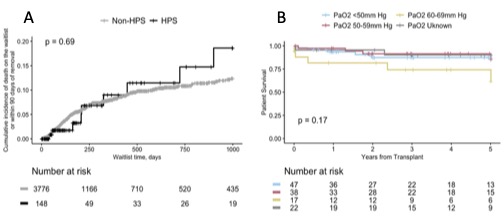
*Results: Among 3,105 pediatric liver transplant recipients included in the study, 124 patients (4%) received MELD/PELD exceptions for HPS. Patients with HPS were median 9 [IQR 6, 12] years old, 54.8% female, and 54% Caucasian. Most patients (87.9%) were listed with a lab MELD/PELD<15. Waitlist mortality was rare and not different for HPS vs non-HPS patients (Figure 1A; p=0.69). Children with HPS had shorter waiting time (median 70 days [IQR 32, 173]) vs non-HPS patients (91 days [IQR 42, 202], p=0.03). When stratified by pre-LT PaO2, hypoxemia was not associated with differences in 1-, 3-, or 5-year survival post-LT (Figure 1B; p=0.17). However, HPS patients experienced slightly lower survival at 5-years compared to non-HPS patients (87.2% vs 92.4%; p=0.04).
*Conclusions: In this large, national analysis of LT outcomes for children with HPS, HPS was not associated with increased risk of waitlist mortality. Children with HPS MELD/PELD exceptions are transplanted quickly and achieve excellent survival post-LT. Severity of pre-LT hypoxemia does not impact post-LT survival. These data suggest that adult criteria for MELD/PELD exceptions may not appropriately capture HPS severity in pediatric patients. Further prospective multicenter studies to examine risk factors in children with HPS are warranted.
To cite this abstract in AMA style:
Raza MH, Kobierski P, Misra A, Lim A, Goldbeck C, Etesami K, Kohli R, Emamaullee J. Meld/Peld Exception Policy and Outcomes in Children with Hepatopulmonary Syndrome Requiring Liver Transplantation in the United States [abstract]. Am J Transplant. 2022; 22 (suppl 3). https://atcmeetingabstracts.com/abstract/meld-peld-exception-policy-and-outcomes-in-children-with-hepatopulmonary-syndrome-requiring-liver-transplantation-in-the-united-states/. Accessed February 22, 2026.« Back to 2022 American Transplant Congress