Lung Transplantation After Ex-Vivo Lung Perfusion versus Static Cold Storage: A Single Institution Cost Analysis
1Duke University School of Medicine, Durham, NC, 2Surgery, Duke University Medical Center, Durham, NC, 3Office of Finance, Duke Transplant Center, Durham, NC
Meeting: 2021 American Transplant Congress
Abstract number: 1204
Keywords: Economics, Lung preservation, Lung transplantation
Topic: Clinical Science » Lung » Lung: All Topics
Session Information
Session Name: Lung: All Topics
Session Type: Poster Abstract
Session Date & Time: None. Available on demand.
Location: Virtual
*Purpose: Ex-vivo lung perfusion (EVLP) allows for reconditioning of “marginal” lung grafts and extended lung preservation. However, EVLP is costlier than cold storage. We compared perioperative outcomes and index hospitalization costs among matched EVLP and non-EVLP lung transplant (LTx) recipients to explore whether upfront device costs may be offset by reduced postoperative costs.
*Methods: LTx recipients at our institution who received donor lungs that underwent EVLP were eligible for inclusion. Patients without cost data were excluded. A group of non-EVLP bilateral LTx recipients was matched 1:3 (nearest neighbor) based on age at LTx, disease group, lung allocation score, and history of prior LTx. Perioperative outcomes and index hospitalization costs were compared between EVLP and non-EVLP groups using descriptive statistics.
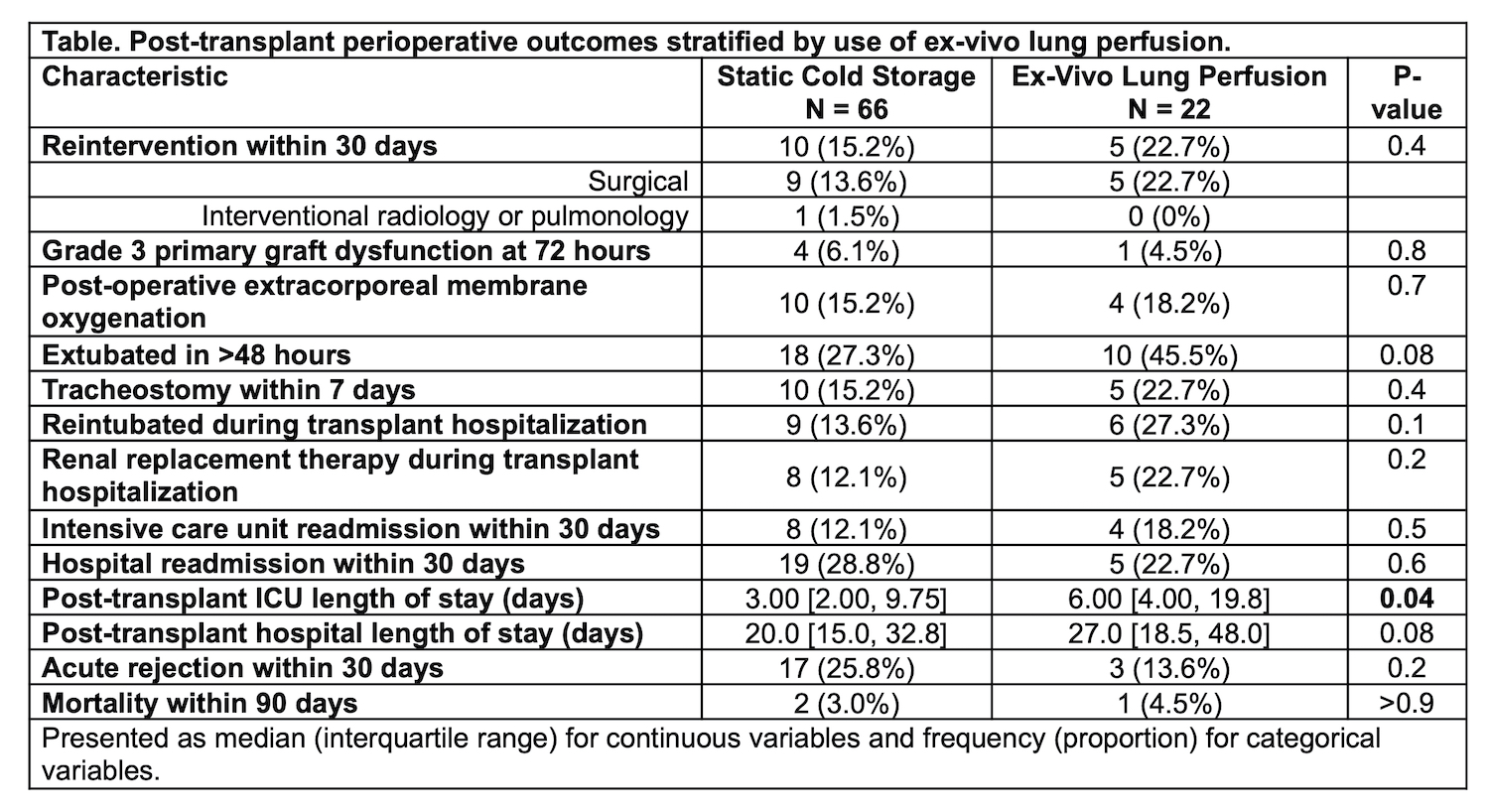
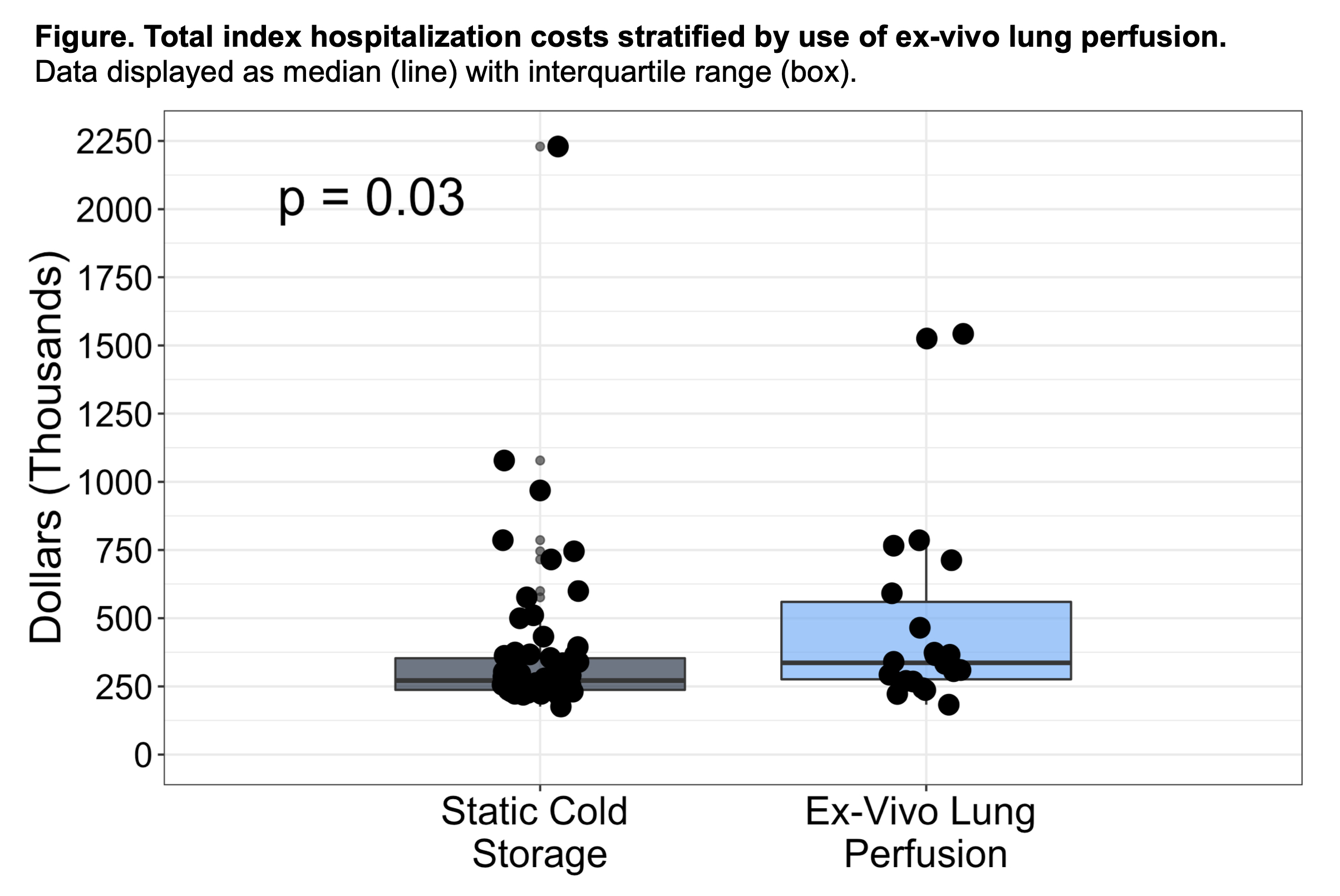
*Results: 22 EVLP and 66 non-EVLP LTx recipients were included. Total preservation time was median 840 vs 415 minutes for EVLP and non-EVLP lungs, respectively (p<0.01). Median EVLP time was 313 minutes. EVLP lungs had lower pre-procurement PaO2/FiO2 ratios than non-EVLP lungs (median 334 vs 444, p<0.01) and were more likely to come from DCD donors (27.3% vs 10.6%, p=0.056). Post-LTx ICU stays were longer among EVLP patients; other outcomes were similar between groups (Table). Excluding device-specific costs, direct variable and total index hospitalization costs were higher among EVLP vs non-EVLP patients (direct variable: median $200,404 vs $157,852, p=0.047; total: median $336,290 vs $271,306, p=0.03) (Figure). EVLP patients incurred higher inpatient pharmacy and diagnostic testing costs than non-EVLP patients, the latter mostly representing bronchoscopies.
*Conclusions: In this institutional analysis, EVLP LTx recipients incurred higher index hospitalization costs than non-EVLP LTx recipients. Further investigation is needed to better understand financial implications of EVLP as a facilitator of donor pool expansion and improved logistics in an era of broader lung sharing.
To cite this abstract in AMA style:
Halpern SE, Kesseli SJ, Au S, Krischak MK, Olaso DG, Smith H, Tipton G, Jamieson I, Haney JC, Klapper JA, Hartwig MG. Lung Transplantation After Ex-Vivo Lung Perfusion versus Static Cold Storage: A Single Institution Cost Analysis [abstract]. Am J Transplant. 2021; 21 (suppl 3). https://atcmeetingabstracts.com/abstract/lung-transplantation-after-ex-vivo-lung-perfusion-versus-static-cold-storage-a-single-institution-cost-analysis/. Accessed February 27, 2026.« Back to 2021 American Transplant Congress