Low HLA Class I Epitope Mismatch Associated with Improved Pancreas Graft Survival in Simultaneous Pancreas-Kidney Transplantation
University of Alabama-Birmingham, Birmingham, AL
Meeting: 2020 American Transplant Congress
Abstract number: 106
Keywords: Epitopes, Histocompatibility antigens, HLA antigens, MHC class I
Session Information
Session Name: Histocompatibility and Immunogenetics
Session Type: Oral Abstract Session
Date: Saturday, May 30, 2020
Session Time: 3:15pm-4:45pm
 Presentation Time: 3:51pm-4:03pm
Presentation Time: 3:51pm-4:03pm
Location: Virtual
*Purpose: Antibody-mediated rejection remains the principal cause of allotransplant graft failure. Human leukocyte antigen (HLA) matching between donor and recipients significantly reduces the risk of kidney organ rejection and failure, but studies differ on the impact of HLA matching in pancreas transplants. We hypothesized that HLA epitope/eplet mismatches (MMs) as determined by the HLA Matchmaker algorithm are a marker for de novo donor specific antibody (dnDSA) development and pancreas graft survival in simultaneous pancreas-kidney transplants.
*Methods: A retrospective chart review of the 210 simultaneous pancreas-kidney (SPK) transplants performed at our institution since Jan 2002 was performed. The National Marrow Donor Program’s HaploStats tool was used to convert donor and recipient low resolution molecular HLA haplotypes to high-resolution alleles and reviewed by a senior member of the HLA Laboratory for accuracy. The HLA-Matchmaker software was used to make predictions of potential MMs between donor-recipient pairs. All statistics were performed in GraphPad Prism software.
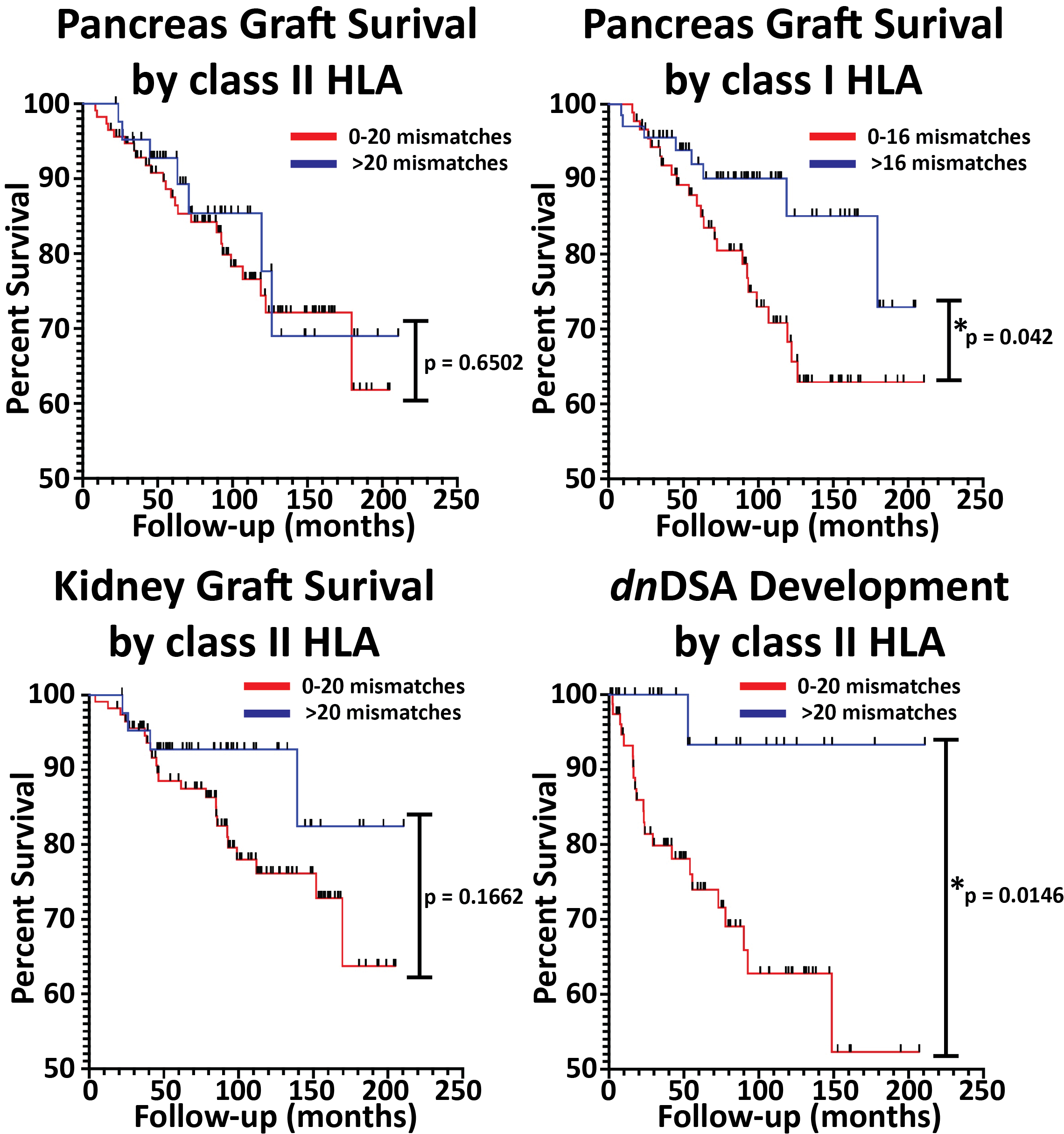
*Results: From the 210 patients, 53 were excluded from analysis for non-immunological complications or lack of sufficient follow-up. During a median follow-up of 89.5 months (8.5 – 210.6 months), 31 patients of the remaining 157 (19.8%) developed pancreas graft failure, 27 developed kidney graft failure (17.2%), and 23 developed dnDSA as measured by single antigen beads (14.6%). Of those with pancreas graft failure, the mean time to graft failure was 64.5 months (range 8.5 – 171.1 months). The effect of HLA MMs on pancreas graft survival using a Kaplan-Meier graft survival curve showed significantly improved pancreas graft survival with HLA class I MM (Figure 1, 0-16 vs ≥17, log-rank test, p = 0.0420), and HLA-A MM (0-7 vs ≥7 MM, p = 0.0437) but not HLA-B (0-4 vs ≥5, p = 0.9248), HLA-C (0-4 vs ≥5, p = 0.8151), class II HLA (0-20 vs ≥ 20 MM, p = 0.6502), HLA-DR (0-9 vs ≥10 MM, p = 0.9554), HLA-DQ (0-16 vs ≥17 MM, p = 0.7306). Freedom from dnDSA development was associated with class II MM (p = 0.0146) but not class I MM (p = 0.2443), while kidney graft survival in the SPK was not associated with class II MM (p = 0.1662) or class I MM (p = 0.9608).
*Conclusions: To the best of our knowledge this is the first time HLAMatchmaker epitopes have been applied to pancreas whole-organ graft survival. Although not associated with dnDSA development, minimizing HLA-A mismatches may positively impact pancreas graft survival.
To cite this abstract in AMA style:
Ladowski JM, Romine M, Kloda D, Young C, Locke J, Hauptfeld-Dolejsek V, Houp J. Low HLA Class I Epitope Mismatch Associated with Improved Pancreas Graft Survival in Simultaneous Pancreas-Kidney Transplantation [abstract]. Am J Transplant. 2020; 20 (suppl 3). https://atcmeetingabstracts.com/abstract/low-hla-class-i-epitope-mismatch-associated-with-improved-pancreas-graft-survival-in-simultaneous-pancreas-kidney-transplantation/. Accessed February 16, 2026.« Back to 2020 American Transplant Congress