Long-Term Outcomes of ATG versus IL-2 Receptor Antagonist in Low Risk Kidney Transplant Recipients: Donor Factors.
JHU, Baltimore
CU, Denver.
Meeting: 2016 American Transplant Congress
Abstract number: 221
Keywords: Immunosuppression, Induction therapy, Kidney transplantation, Outcome
Session Information
Session Name: Concurrent Session: Kidney: Induction Therapy 1
Session Type: Concurrent Session
Date: Monday, June 13, 2016
Session Time: 2:30pm-4:00pm
 Presentation Time: 2:42pm-2:54pm
Presentation Time: 2:42pm-2:54pm
Location: Room 312
Controversy exists regarding the optimal choice of induction therapy in low-risk kidney transplant (KT) recipients. Current guidelines specify induction choices in KT based on recipient factors and would recommend IL2 receptor antagonists over ATG in low-risk patients. However, the impact of donor factors in this decision-making remains unclear. We aimed to compare outcomes of ATG versus IL-2 receptor antagonists in low-risk KT, stratified by Kidney Donor Profile Index (KDPI).
METHODS: Using OPTN data, we identified 14,172 low-risk (first-time, KT alone, non-African American, PRA<20%, HIV-negative, HCV-negative, CIT<24h) deceased-donor KT recipients between 2003-2014 who received ATG or IL2 induction in addition to Tacrolimus (Tac), Mycophenolate (MPA), and steroid immunosuppression. We built Cox models for all-cause graft loss (ACGL), death-censored graft loss (DCGL), and mortality, as well as logistic regression models for acute rejection at 1 year (AR). Patients were stratified into 3 KDPI categories (low: 0-34, moderate: 35-85, high: 86+)
| Table 1: KDPI Strata |
ATG (N=7862) |
IL2 (N=6310) |
| Low 0-34 | 30.6% | 38.4% |
| Moderate 35-85 | 57.8% | 53.6% |
| High 86+ | 11.5% | 8.0% |
.
RESULTS: Compared to ATG, IL2 in low, moderate, and high-KDPI KT was not associated with a difference in ACGL (aHR=0.850.981.11, p=0.7, 0.890.981.07, p=0.6, and0.740.891.07, p=0.2), DCGL (aHR=0.770.951.17, p=0.6, 0.891.031.20, p=0.6,and0.690.921.23, p=0.6), or mortality (aHR=0.840.981.15, p=0.8, 0.840.931.04, p=0.2, and0.740.901.10, p=0.3). However, IL2 was associated with increased risk of AR in moderate-KDPI KT (aOR= 1.061.261.56, p=0.01) and high-KDPI KT (aOR= 1.161.642.32, p=0.01), but not low-KDPI KT (aOR= 0.740.961.30, p=0.76) 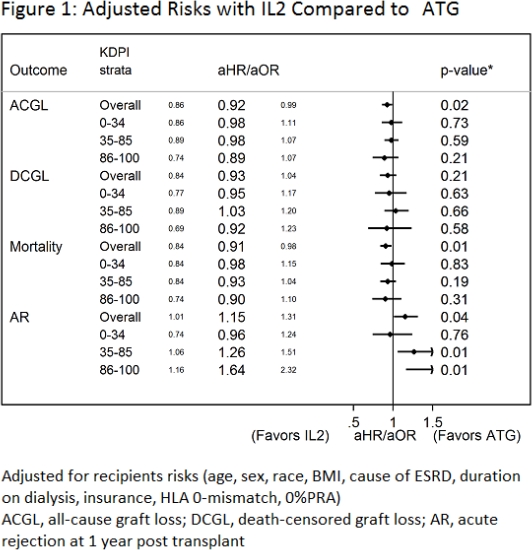 .
.
CONCLUSION: ATG was not associated with superior long-term benefits compared to IL2 within all KDPI strata when using Tac/MPA/prednisone in a low-risk KT population, while the risk of AR was similar in the low-KDPI category. These results suggest that KDPI can be used to guide selecting the optimal induction therapy in otherwise low-risk KT recipients.
CITATION INFORMATION: Al Ammary F, Bae S, Massie A, Desai N, Dagher N, Kraus E, Wiseman A, Segev D. Long-Term Outcomes of ATG versus IL-2 Receptor Antagonist in Low Risk Kidney Transplant Recipients: Donor Factors. Am J Transplant. 2016;16 (suppl 3).
To cite this abstract in AMA style:
Ammary FAl, Bae S, Massie A, Desai N, Dagher N, Kraus E, Wiseman A, Segev D. Long-Term Outcomes of ATG versus IL-2 Receptor Antagonist in Low Risk Kidney Transplant Recipients: Donor Factors. [abstract]. Am J Transplant. 2016; 16 (suppl 3). https://atcmeetingabstracts.com/abstract/long-term-outcomes-of-atg-versus-il-2-receptor-antagonist-in-low-risk-kidney-transplant-recipients-donor-factors/. Accessed February 27, 2026.« Back to 2016 American Transplant Congress
