Living versus Deceased Donor Liver Transplantation in Cholestatic Liver Disease: An Analysis of the OPTN Database
1Vanderbilt University Medical Center, Nashville, TN, 2University of Washington, Seattle, WA
Meeting: 2020 American Transplant Congress
Abstract number: D-128
Keywords: Brain death, Liver grafts, Liver transplantation, Living donor
Session Information
Session Name: Poster Session D: Liver: Living Donors and Partial Grafts
Session Type: Poster Session
Date: Saturday, May 30, 2020
Session Time: 3:15pm-4:00pm
 Presentation Time: 3:30pm-4:00pm
Presentation Time: 3:30pm-4:00pm
Location: Virtual
*Purpose: The current MELD allocation system does not accurately reflect the urgency of liver transplantation (LT) in cholestatic liver disease (CLD) patients. Therefore, more CLD patients are waitlisted than transplanted annually. The utilization of living donor LT (LDLT) grafts or donation after circulatory death (DCD) can expand the deceased donor LT (DDLT) pool. We sought to compare the outcomes of donation after brain death [DBD] vs. DCD vs. LDLT in CLD patients.
*Methods: Retrospective cohort analysis of adult CLD primary LT recipients registered in the OPTN database (2002-2018). Cox proportional hazards regression models with mixed effects were used to determine the impact of donor type on patient and graft survival.
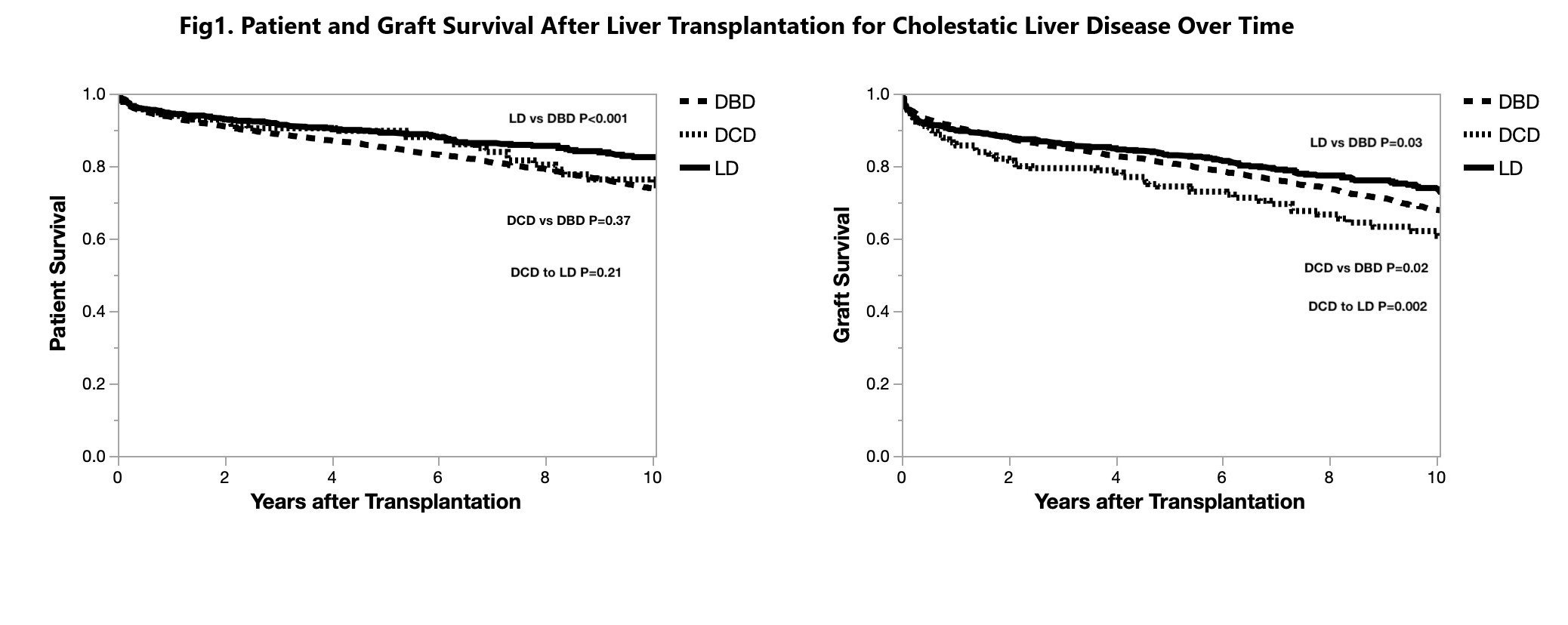
*Results: 5,999 DDLT (5,730 DBD, 269 DCD) and 912 LDLT recipients were identified. DDLT recipients were more commonly older, white, with higher MELD scores, hospitalized or in ICU, mechanically-assisted, and on dialysis at the time of LT when compared to LDLT recipients (all P<0.001). 1-,3-,5-,10-year patient (DBD: 93.6%, 88.8%, 85.1%, 73.8% vs. DCD: 93.9%, 90.4%, 89.7%, 74.7% vs. LDLT: 94.5%, 90.4%, 89.7%, 82.5%), and graft survival rates (DBD: 90.2%, 85.2%, 80.8%, 67.9% vs. DCD: 86.3%, 79.4%, 74.4%, 60.7% vs. LDLT: 89.3%, 86.1%, 83.0%, 73.9%) were superior in the LDLT arm (Fig.1). Higher rates of biliary complications as a cause of graft failure were seen in DCD (56.8%) than LDLT (30.5%) or DBD (18.7%) recipients. On multivariable Cox analysis, recipient diabetes mellitus, hospital or ICU location, previous abdominal surgery, cold ischemia time, donor age, and race were independent predictors of patient mortality and graft failure. On multivariable Cox analysis, donor type was not associated with patient mortality, but DCD was independently associated with graft failure (RR:1.34, 95%CI: 1.18-1.79, P = 0.046).
*Conclusions: LDLT is an optimal alternative to DDLT for CLD patients with superior survival. DCD is an alternative option with acceptable patient survival but inferior graft survival, likely related to the high rate of biliary complications.
To cite this abstract in AMA style:
Ziogas IA, Alexopoulos SP, Matsuoka LK, Geevarghese SK, Gorden LD, Karp SJ, Perkins JD, Montenovo MI. Living versus Deceased Donor Liver Transplantation in Cholestatic Liver Disease: An Analysis of the OPTN Database [abstract]. Am J Transplant. 2020; 20 (suppl 3). https://atcmeetingabstracts.com/abstract/living-versus-deceased-donor-liver-transplantation-in-cholestatic-liver-disease-an-analysis-of-the-optn-database/. Accessed February 16, 2026.« Back to 2020 American Transplant Congress