Kidney Nonprocurement in Deceased Donors with Acute Kidney Injury
1Division of Nephrology, Columbia University Medical Center, New York, NY, 2Division of Nephrology, Johns Hopkins School of Medicine, Baltimore, MD
Meeting: 2022 American Transplant Congress
Abstract number: 399
Keywords: Kidney transplantation, Procurement, Renal injury, Resource utilization
Topic: Clinical Science » Kidney » 32 - Kidney Deceased Donor Selection
Session Information
Session Name: Kidney Deceased Donor Selection II
Session Type: Rapid Fire Oral Abstract
Date: Tuesday, June 7, 2022
Session Time: 3:30pm-5:00pm
 Presentation Time: 4:50pm-5:00pm
Presentation Time: 4:50pm-5:00pm
Location: Hynes Ballroom C
*Purpose: Deceased donor acute kidney injury (AKI) is associated with high rates of kidney discard by transplant centers, despite evidence of excellent post-transplant outcomes. High discard rates may consequently drive nonprocurement of these kidneys by OPOs. We aimed to study the relationship between donor AKI and kidney nonprocurement.
*Methods: We used OPTN STAR and DonorNet data to identify deceased donors with ≥1 solid organ (i.e. kidney, liver, lung, or heart) recovered for transplantation from 2008-2018. Donor AKI was staged using KDIGO criteria based on the minimum and maximum creatinine during hospitalization. We compared characteristics of donors with no kidneys procured across no AKI vs stage 1 vs 2 vs 3. We used multivariable logistic regression to analyze the relationship between AKI severity and kidney nonprocurement after adjusting for donor characteristics.
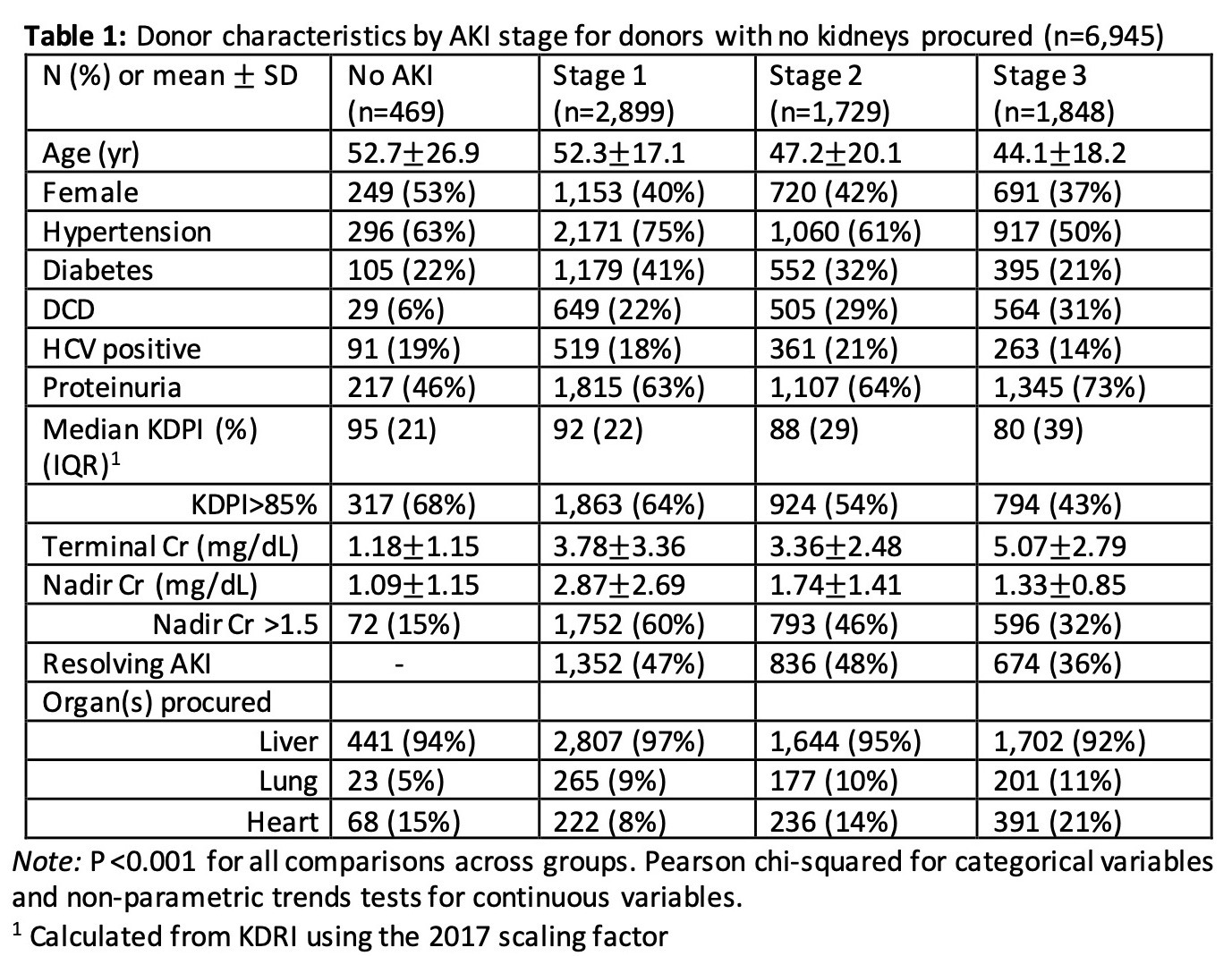
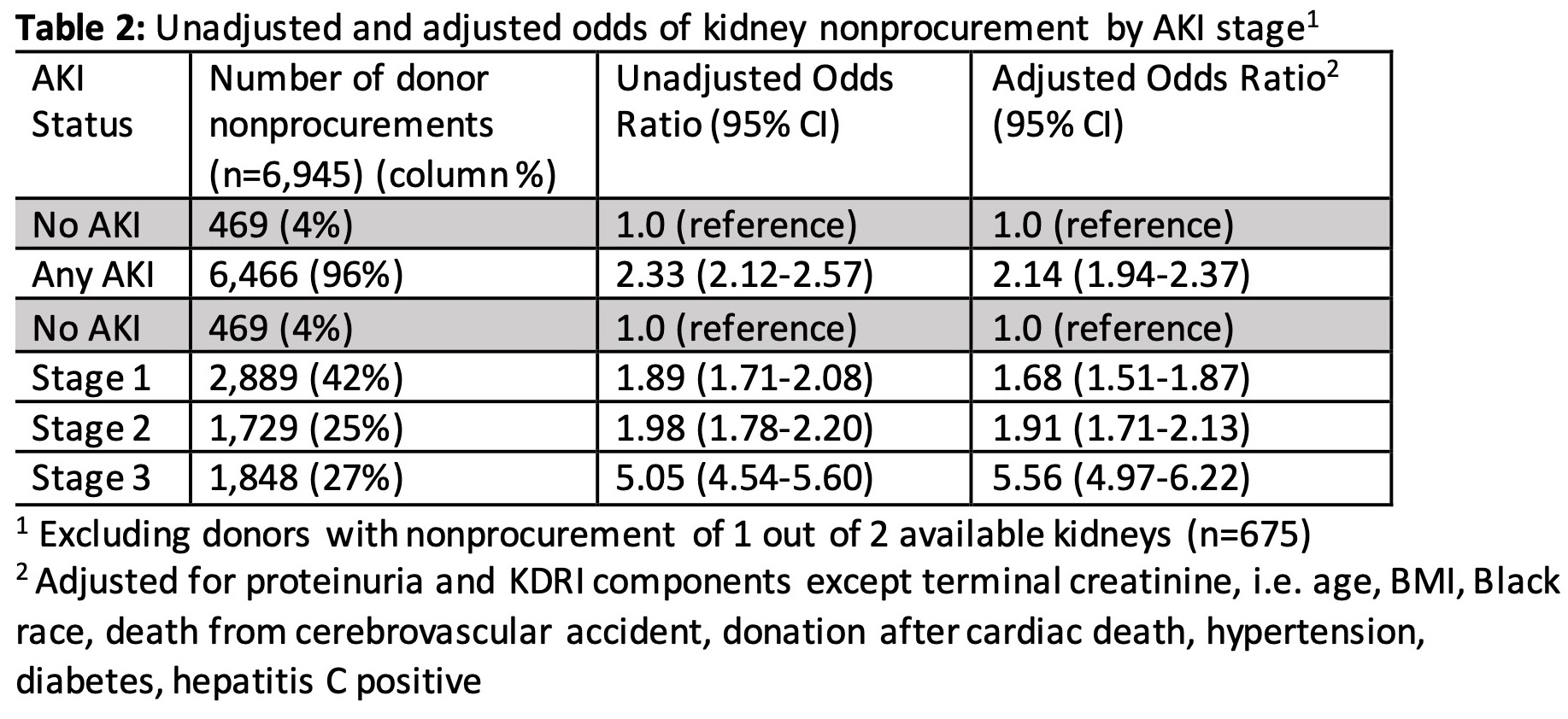
*Results: A total of 14,543 kidneys (mean 1,314 per year) from 7,620 donors were not procured over the 11-year study period. The majority of nonprocured kidneys (13,497 kidneys, 93%) were from donors with AKI. Among 6,945 donors (7%) with no kidneys procured but a liver, lung, and/or heart recovered, the plurality had stage 1 (42%), followed by stage 3 (27%), stage 2 (25%), and no AKI (7%) (Table 1). Donors with stage 3 AKI were the youngest and least likely to be hypertensive, diabetic, or HCV+, compared to donors with no AKI or lesser AKI stages (P<0.001). They had the lowest KDPI and highest rates of heart and lung procurements among any group (P<0.001). Adjusted odds of kidney nonprocurement ranged from 1.68 (95%CI 1.51-1.87) for stage 1 to 5.56 for stage 3 AKI (95%CI 4.97-6.22), compared to donors with no AKI (Table 2).
*Conclusions: The majority of kidney nonprocurements in deceased donors occurred in the setting of donor AKI. AKI severity is a strong risk factor for kidney nonprocurement, despite procurement of extrarenal organs from these donors. Optimizing safe procurement and utilization of kidneys from donors with AKI should be a focus of efforts to address the organ shortage given the excellent post-transplant outcomes with these kidneys.
To cite this abstract in AMA style:
Yu K, King K, Husain S, Stevens J, Parikh C, Mohan S. Kidney Nonprocurement in Deceased Donors with Acute Kidney Injury [abstract]. Am J Transplant. 2022; 22 (suppl 3). https://atcmeetingabstracts.com/abstract/kidney-nonprocurement-in-deceased-donors-with-acute-kidney-injury/. Accessed February 27, 2026.« Back to 2022 American Transplant Congress