Kidney Grafts From Donors After Circulatory Death Provide Comparable Outcome To Donors After Brain Death Without Intracorporeal In Situ Cooling
Sapporo City General Hospital, Sapporo, Hokkaido, Japan
Meeting: 2019 American Transplant Congress
Abstract number: A201
Keywords: Allocation, Donors, non-heart-beating, Survival
Session Information
Session Name: Poster Session A: Kidney Deceased Donor Allocation
Session Type: Poster Session
Date: Saturday, June 1, 2019
Session Time: 5:30pm-7:30pm
 Presentation Time: 5:30pm-7:30pm
Presentation Time: 5:30pm-7:30pm
Location: Hall C & D
*Purpose: Donation after circulatory death (DCD) had been one and only source of deceased kidney donor in our country. The number of donation after brand death (DBD) is increasing after the launch of law of DBD in 1997. The number of DBD transplant has increased after the amendment of allocation rule (national shipment to regional shipment) in 2002. In contrast, ironically the number of DCD dramatically decreased year by year. To remind the less inferiority of graft quality compared to DBD and resilient the donation, we herein survey the outcome of DCD kidney transplant in our region.
*Methods: Eighty-three kidney recipients accepted from deceased donors in our region (Hokkaido block) from 1999 were enrolled in this study. They were divided into two groups according to era. In Era I (n=19), kidney transplants were performed before 2002 some grafts were shipped from other blocks. In Era II (n=64), kidney grafts were donated only in our block. The ratio of DBD/DCD were somewhat different between two eras (2:17 vs. 20:44, respectively, p=0.0838), total ischemic time is longer in Era I (mean 906.7 vs. 458.5, respectively, p<0.0001) and recipient age is younger in Era I (mean 41.0 vs. 51.3, p=0.0002). Other factors (donor age, sex, in-situ cannulation, recipient sex, primary non- function rate, DGF period) were comparable between two groups. We first compare the graft survival between two eras. Next, we compared the graft survival in Era II. Finally, we compared the graft survival according to pre-procurement in-situ cannulation for in-situ cooling or not in Era II.
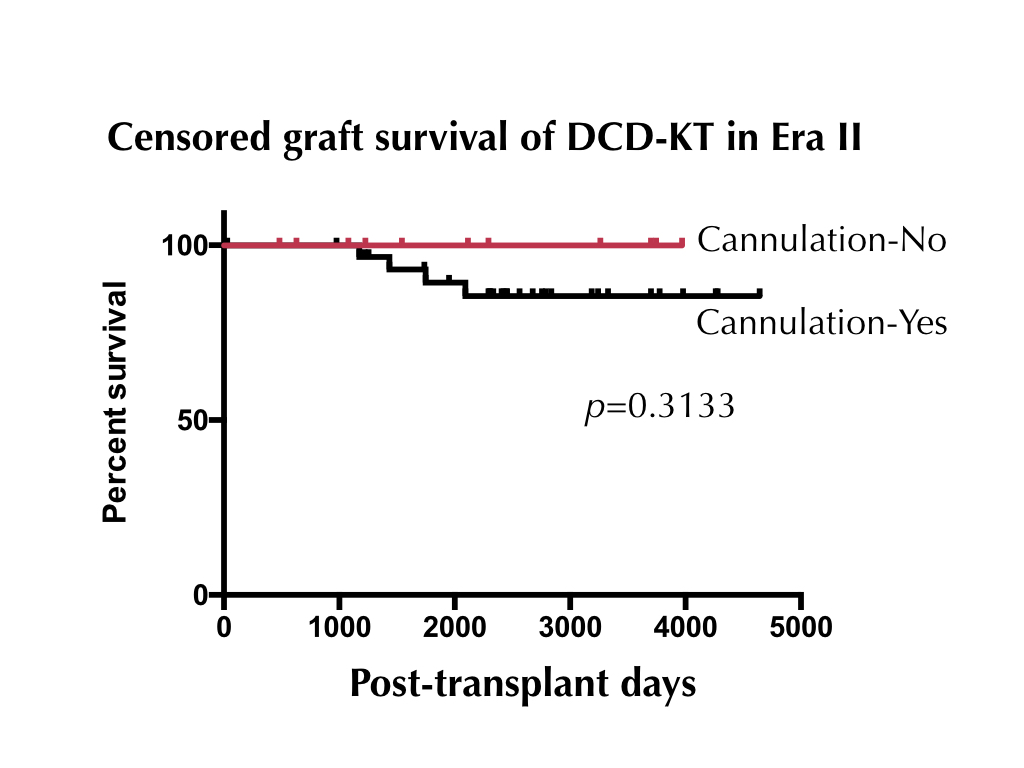
*Results: Non-censored graft survival in Era II was somewhat better compared to Era I (p=0.0737). Although, censored graft survival was similar between two eras (p=0.2718). out of 131 Censored graft survivals between DCD and DBD were completely comparable in Era II (p=1.000). Interestingly, organ procurements without in-situ cannulation did not impaired graft survival compared to that from without pre-procurement cannulation (p=0.3133) (Figure).
*Conclusions: The outcome of kidney transplant from DCD is completely comparable to from DBD under the regional shipment policy. We should encourage and revisit DCD donor expansion even without pre-procurement in-situ cannulation to fill up organ shortage in our living donation oriented country.
To cite this abstract in AMA style:
Harada H, Miura M, Mitsuke A, Higuchi H, Fukuzawa N, Tanaka H, Hirano T, Seki T. Kidney Grafts From Donors After Circulatory Death Provide Comparable Outcome To Donors After Brain Death Without Intracorporeal In Situ Cooling [abstract]. Am J Transplant. 2019; 19 (suppl 3). https://atcmeetingabstracts.com/abstract/kidney-grafts-from-donors-after-circulatory-death-provide-comparable-outcome-to-donors-after-brain-death-without-intracorporeal-in-situ-cooling/. Accessed July 3, 2025.« Back to 2019 American Transplant Congress