Kidney Allograft Loss After Simultaneous Liver Kidney (SLK) Transplant Before and After the New SLK Allocation Criteria Implementation
1Medicine, University of Minnesota, Minneapolis, MN, 2Analytics, Mhealth-Fairview, Minneapolis, MN
Meeting: 2022 American Transplant Congress
Abstract number: 1083
Keywords: Allocation, Graft survival, Kidney/liver transplantation, Multivisceral transplantation
Topic: Clinical Science » Liver » 52 - Liver: Kidney Issues in Liver Transplantation
Session Information
Session Name: Liver: Kidney Issues in Liver Transplantation
Session Type: Poster Abstract
Date: Sunday, June 5, 2022
Session Time: 7:00pm-8:00pm
 Presentation Time: 7:00pm-8:00pm
Presentation Time: 7:00pm-8:00pm
Location: Hynes Halls C & D
*Purpose: On August 10, 2017 UNOS/OPTN implemented new allocation criteria for simultaneous liver-kidney (SLK) transplants. We sought to examine the association between the new allocation criteria and the short-term kidney graft outcome.
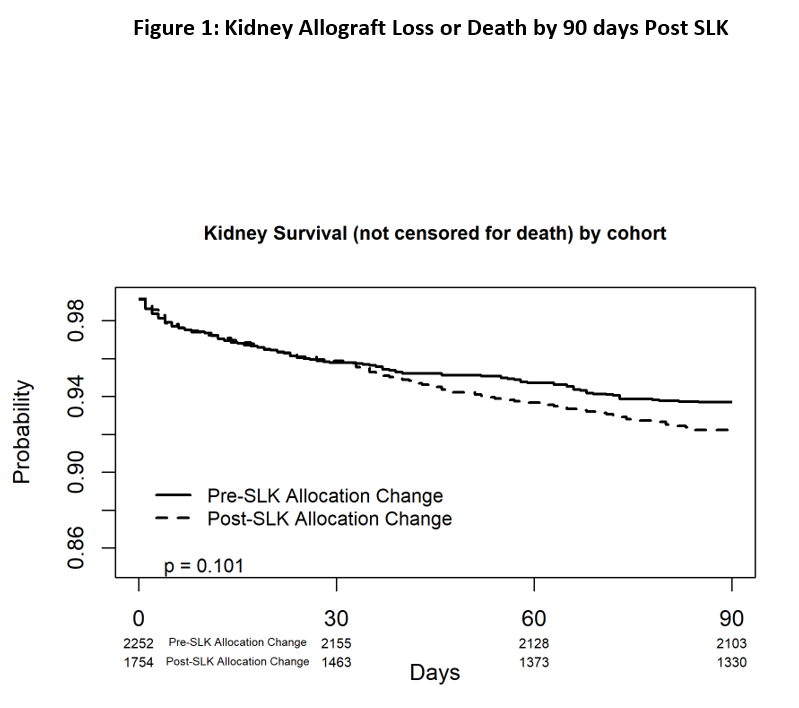
*Methods: Utilizing the Scientific Registry of Transplant Recipients (SRTR) standard analysis file, we identified all adult primary SLK recipients transplanted between Jan 1, 2014-August 9, 2017 (pre SLK allocation change) and those both listed and transplanted between August 10, 2017-September 1, 2020 (post SLK allocation change). We compared baseline characteristics of SLK recipients pre (n=2252) and post (n=1754) allocation change and compared short term outcomes. A Kaplan-Meier curve was generated for kidney allograft failure or death by 90 days post-transplant between groups. Cox proportional hazard model was used to examine the association between the new allocation criteria and all cause kidney graft loss by 90 days. The model was adjusted for recipient age, sex, BMI, diabetes status, ethnicity, on dialysis, in ICU at time of transplant, MELD, portal vein thrombosis, liver transplant indication, HCV infection, donor age, donor sex, kidney CIT, DCD, donor height, and organ importation status.
*Results: Nonalcoholic steatohepatitis as an indication for transplantation increased from 22.4% to 31.2% and viral hepatitis decreased from 27.2% to 14.3% post allocation change. There was an increase in imported organ use from 34.1% to 43.3%. There were no differences in short term outcome. In the Kaplan-Meier analysis there was no difference in kidney allograft survival or death by 90 days after the allocation change (Figure 1). In the multivariable Cox proportional hazard analysis allocation change was not associated with kidney graft loss or death by 90 days (LLCI, aHR, ULCI) (0.9, 1.17, 1.51). Being in the ICU at time of transplant, on dialysis prior to transplant, older donor age, longer kidney CIT, were deleterious predictors, however increased donor height was a favorable predictor of kidney graft loss or death by 90 days.
*Conclusions: The new SLK allocation scheme did not seem to influence kidney allograft loss or death by 90 days. Identifying deleterious predictors of kidney graft loss or death by 90 days post SLK may improve the appropriateness of kidney utilization in SLK.
To cite this abstract in AMA style:
Bregman AP, Jackson S, Lim N, Lake J, Riad S. Kidney Allograft Loss After Simultaneous Liver Kidney (SLK) Transplant Before and After the New SLK Allocation Criteria Implementation [abstract]. Am J Transplant. 2022; 22 (suppl 3). https://atcmeetingabstracts.com/abstract/kidney-allograft-loss-after-simultaneous-liver-kidney-slk-transplant-before-and-after-the-new-slk-allocation-criteria-implementation/. Accessed February 22, 2026.« Back to 2022 American Transplant Congress