Ischemia Reperfusion Injury & Risk for Antibody Mediated Rejection (ABMR) in HLA Sensitized Patients Treated with C1 Esterase Inhibitor (C1INH)
1Kidney Transplant, Cedars-Sinai Medical Center, LA, CA
2Paris Translational Research for Organ Transplantation, Necker Hospital, Paris, France.
Meeting: 2018 American Transplant Congress
Abstract number: 19
Keywords: Glomerular filtration rate (GFR), Highly-sensitized, Ischemia, Kidney transplantation
Session Information
Session Name: Concurrent Session: Kidney Acute Antibody Mediated Rejection
Session Type: Concurrent Session
Date: Sunday, June 3, 2018
Session Time: 2:30pm-4:00pm
 Presentation Time: 2:30pm-2:42pm
Presentation Time: 2:30pm-2:42pm
Location: Room Hall 4B
Introduction: Ischemia reperfusion injury (IRI) contributes to delayed graft function (DGF). IRI/DGF in HLA-sensitized (HS) patients likely activates innate and memory injury pathways that may contribute to poor outcomes. C1INH is a serpin (serine protease inhibitor) that inhibits the classic and mannose binding lectin/mannose associated serine protease pathways (MBL/MASP). Here we report outcomes of a Phase I/II placebo-controlled study investigating the safety & efficacy of C1INH to reduce DGF in a cohort of HS patients receiving DD kidney transplants after desensitization. (NCT#02134314). Patients & Methods: From November 2014- February 2017, 70 HS & Non-HS patients were enrolled & randomized 1:1 to receive C1INH 50U/kg (n=35) vs. Placebo (n=35) intra-operatively & 24hrs later. Of the 70 patients, 17 were HLA sensitized and their outcomes are analyzed here. Results: Seventeen HS patients with risks for DGF were randomized: {G1:C1INH (n=10) vs. G2:Placebo (n=7)}. Briefly, CPRA 99-100% & previous transplants were equivalent in G1 & G2. Pre-implantation biopsies were similar. Though not significant, need for dialysis @3-4 weeks post-transplant was 0% (G1) vs. 26% (G2) {Fig 1}. ABMR+TG occurred in 2 patients (20%) in G1 @16M & @30M. In G2, ABMR+TMA occurred in 1 patient @<1M and in another patient, dnDSA induced ABMR occurred @6M post-transplant. No graft loss (0%) occurred in G1, but 2 (29%) occurred in G2 {BKAN (1), ABMR (1)}. No significant differences in eGFR @12M & 24M were seen, G1: 65±21 & 65±12 vs. G2: 55±3 & 50±16 (P=NS) {Fig 2}. 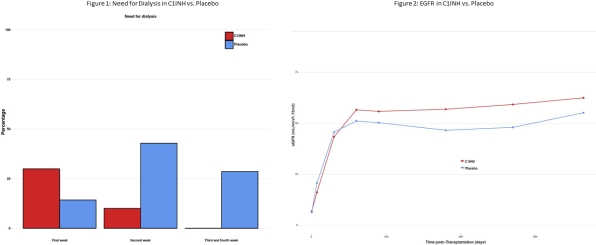 Conclusions: C1INH appeared to offer a benefit in HS patients (CPRA 99-100%) in protecting patients from early ABMR associated graft loss. Though not significant, need for dialysis @3-4 weeks as well as renal function @12M & 24M post transplant were numerically superior in C1INH treated group. Therefore, prevention strategies with emphasis on therapeutic targets could improve long-term outcomes in patients w. IRI/DGF.
Conclusions: C1INH appeared to offer a benefit in HS patients (CPRA 99-100%) in protecting patients from early ABMR associated graft loss. Though not significant, need for dialysis @3-4 weeks as well as renal function @12M & 24M post transplant were numerically superior in C1INH treated group. Therefore, prevention strategies with emphasis on therapeutic targets could improve long-term outcomes in patients w. IRI/DGF.
CITATION INFORMATION: Vo A., Aubert O., Choi J., Ammerman N., Edmund H., Peng A., Najjar R., Supreet S., Jordan S. Ischemia Reperfusion Injury & Risk for Antibody Mediated Rejection (ABMR) in HLA Sensitized Patients Treated with C1 Esterase Inhibitor (C1INH) Am J Transplant. 2017;17 (suppl 3).
To cite this abstract in AMA style:
Vo A, Aubert O, Choi J, Ammerman N, Edmund H, Peng A, Najjar R, Supreet S, Jordan S. Ischemia Reperfusion Injury & Risk for Antibody Mediated Rejection (ABMR) in HLA Sensitized Patients Treated with C1 Esterase Inhibitor (C1INH) [abstract]. https://atcmeetingabstracts.com/abstract/ischemia-reperfusion-injury-risk-for-antibody-mediated-rejection-abmr-in-hla-sensitized-patients-treated-with-c1-esterase-inhibitor-c1inh/. Accessed February 27, 2026.« Back to 2018 American Transplant Congress
