Is Total Ischemic Time a Measure of OPTN Efficiency? Monitoring the Impact of Lung Allocation Policy on Ischemic Time
1United Network for Organ Sharing, Richmond, VA, 2Health Administration, Trinity University, San Antonio, TX
Meeting: 2020 American Transplant Congress
Abstract number: B-283
Keywords: Lung, Monitoring, Multivariate analysis, Public policy
Session Information
Session Name: Poster Session B: Lung: All Topics
Session Type: Poster Session
Date: Saturday, May 30, 2020
Session Time: 3:15pm-4:00pm
 Presentation Time: 3:30pm-4:00pm
Presentation Time: 3:30pm-4:00pm
Location: Virtual
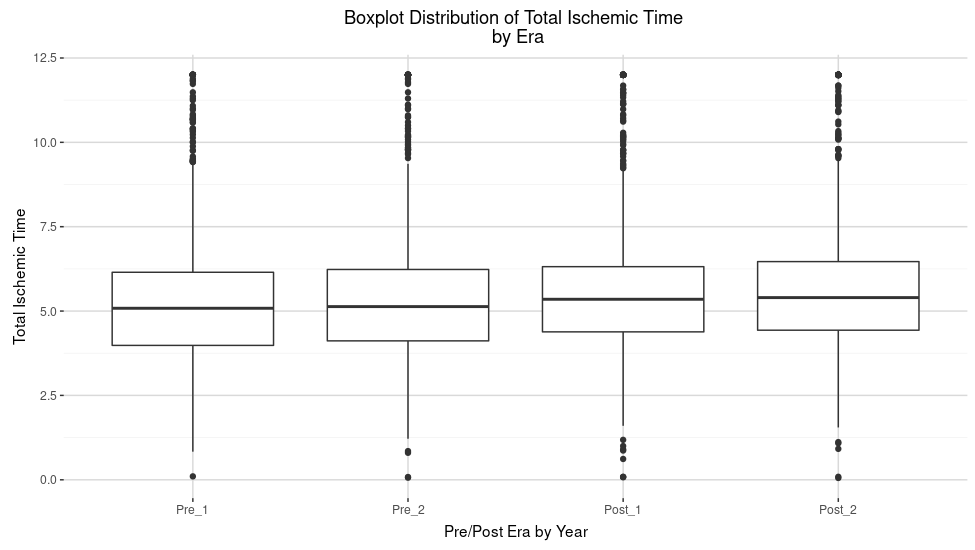
*Purpose: There is concern that the shift to circle based organ allocation policy may increase coordination costs. Within both public comment and the peer reviewed literature, the increase in total ischemic time has been associated with increased coordination costs due to increasingly complex logistical coordination. The prevailing argument is that transplant centers have interacted with more and increasingly distant organ procurement organizations. However, it is of interest to determine if increased total ischemic time is solely driven by logistical coordination stemming from the policy change or other exogenous factors.
*Methods: We developed a dataset at the transplant center level capturing clinical, logistical, and network factors from 2015 to 2019 for all deceased lung transplants within continuous United States. We leveraged a multi-level regression, regressing center level average total ischemic time on transplant centered clinical, logistical, and network data.
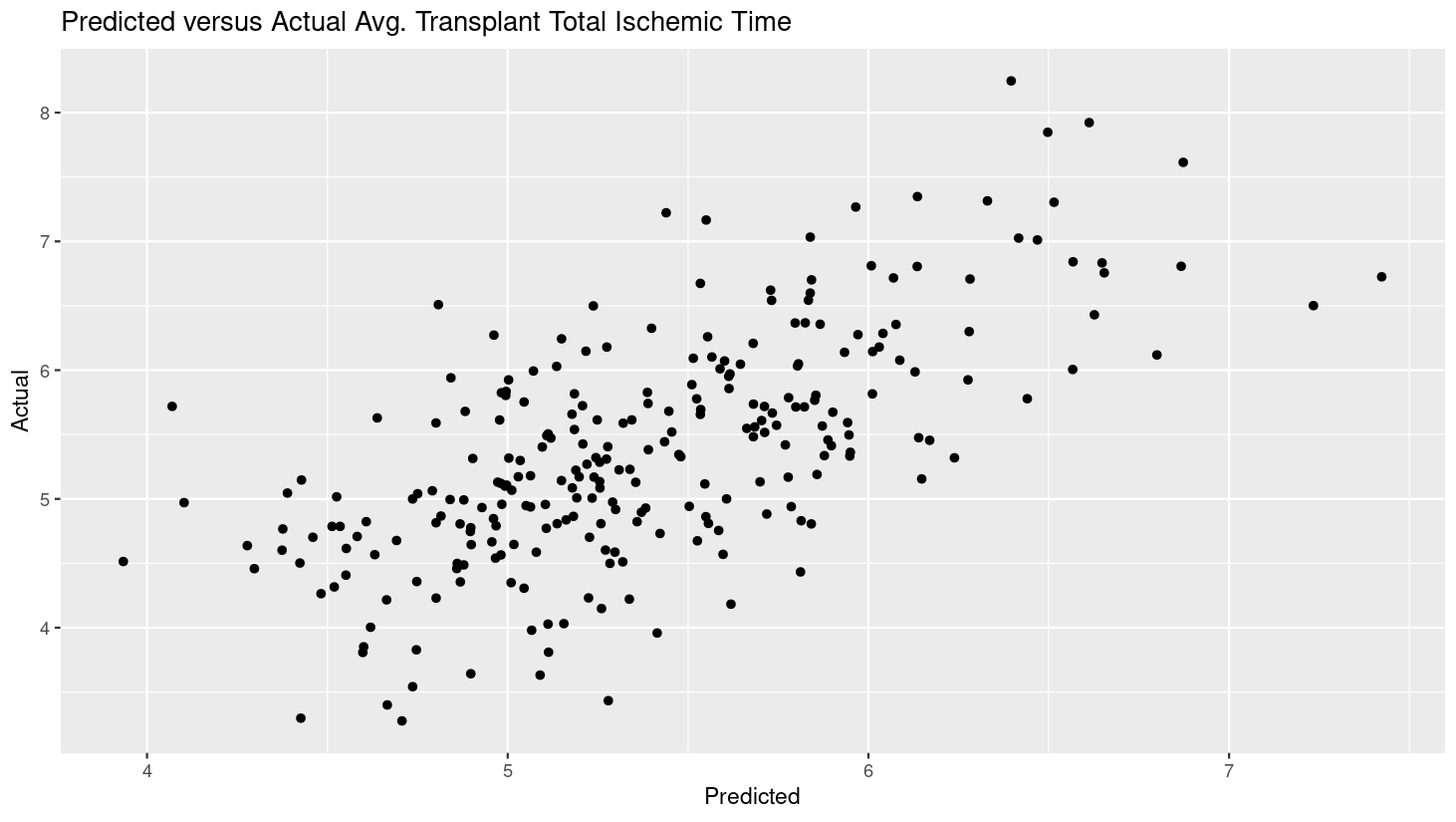
*Results: Our model explains 67% of the variation (r-squared) of total ischemic time compared to 12% of the variation using a model solely based on distance. Statistically significant factors include distance, % of procurements at night, % of single versus double lung transplants, and % of lungs perfused in addition to policy era effects.
*Conclusions: We have demonstrated that logistical, clinical factors, and network factors are statistically significant, which explain five times the variance in total ischemic time than distance alone. Exogenous clinical factors, such as percentage of lungs perfused and percentage of DCD lungs, affect total ischemic time. Hence, the resultant model suggests that leveraging total ischemic time as a measure of network efficiency is more complicated than previously thought.
To cite this abstract in AMA style:
Placona AM, Goff RR, Shay P, Carrico B. Is Total Ischemic Time a Measure of OPTN Efficiency? Monitoring the Impact of Lung Allocation Policy on Ischemic Time [abstract]. Am J Transplant. 2020; 20 (suppl 3). https://atcmeetingabstracts.com/abstract/is-total-ischemic-time-a-measure-of-optn-efficiency-monitoring-the-impact-of-lung-allocation-policy-on-ischemic-time/. Accessed February 27, 2026.« Back to 2020 American Transplant Congress