Is Azathioprine the Right Choice in De Novo Lung Transplantation?
1Pharmacy, University of Utah Health, Salt Lake City, UT, 2Nephrology, University of Utah Health, Salt Lake City, UT, 3Pulmonary, University of Utah Health, Salt Lake City, UT
Meeting: 2020 American Transplant Congress
Abstract number: C-305
Keywords: Bacterial infection, Immunosuppression, Lung transplantation, Rejection
Session Information
Session Name: Poster Session C: Lung: All Topics
Session Type: Poster Session
Date: Saturday, May 30, 2020
Session Time: 3:15pm-4:00pm
 Presentation Time: 3:30pm-4:00pm
Presentation Time: 3:30pm-4:00pm
Location: Virtual
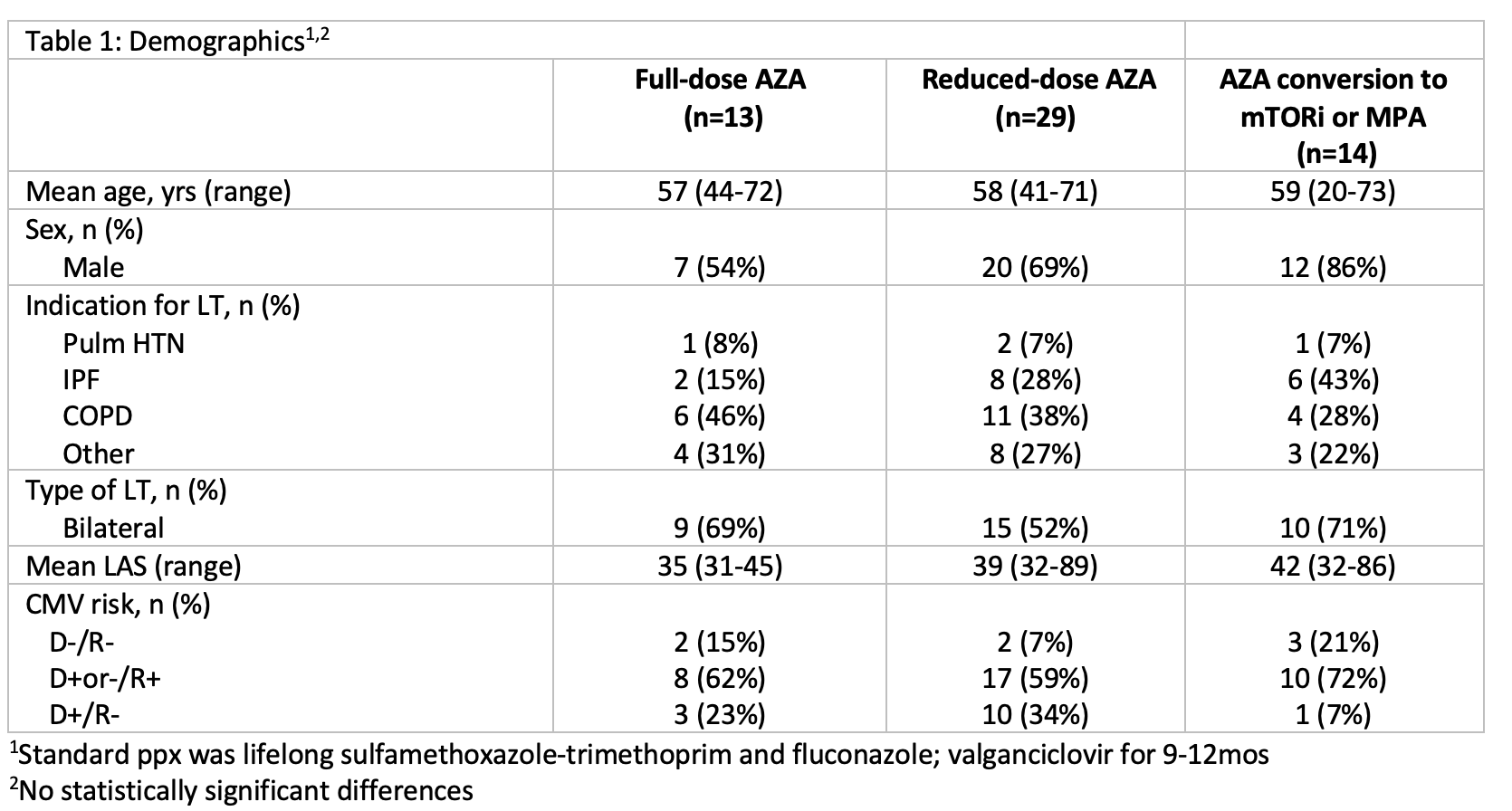
*Purpose: The antiproliferative of choice in lung transplantation (LT) remains controversial. Limited data exists on azathioprine (AZA) dose reductions or the conversion of AZA to mammalian target of rapamycin inhibitor (mTORi) or mycophenolic acid (MPA). We evaluated whether full-dose AZA, reduced-dose AZA, or AZA conversion to an mTORi or MPA affects rejection, graft failure, or mortality when used in combination with tacrolimus and steroids after basiliximab induction.
*Methods: This single center, 1yr, retrospective, descriptive study included pts who received a LT between Jan 2013 and Sep 2018. Full-dose was AZA maintained at 2 mg/kg/day; reduced-dose was any AZA dose reduction; AZA conversion was a change from AZA to an mTORi or MPA. Primary outcomes were rejection, graft failure, and mortality. Secondary outcomes were indication for AZA dose reduction or conversion to an mTORi or MPA, infxns, and change in FEV1.
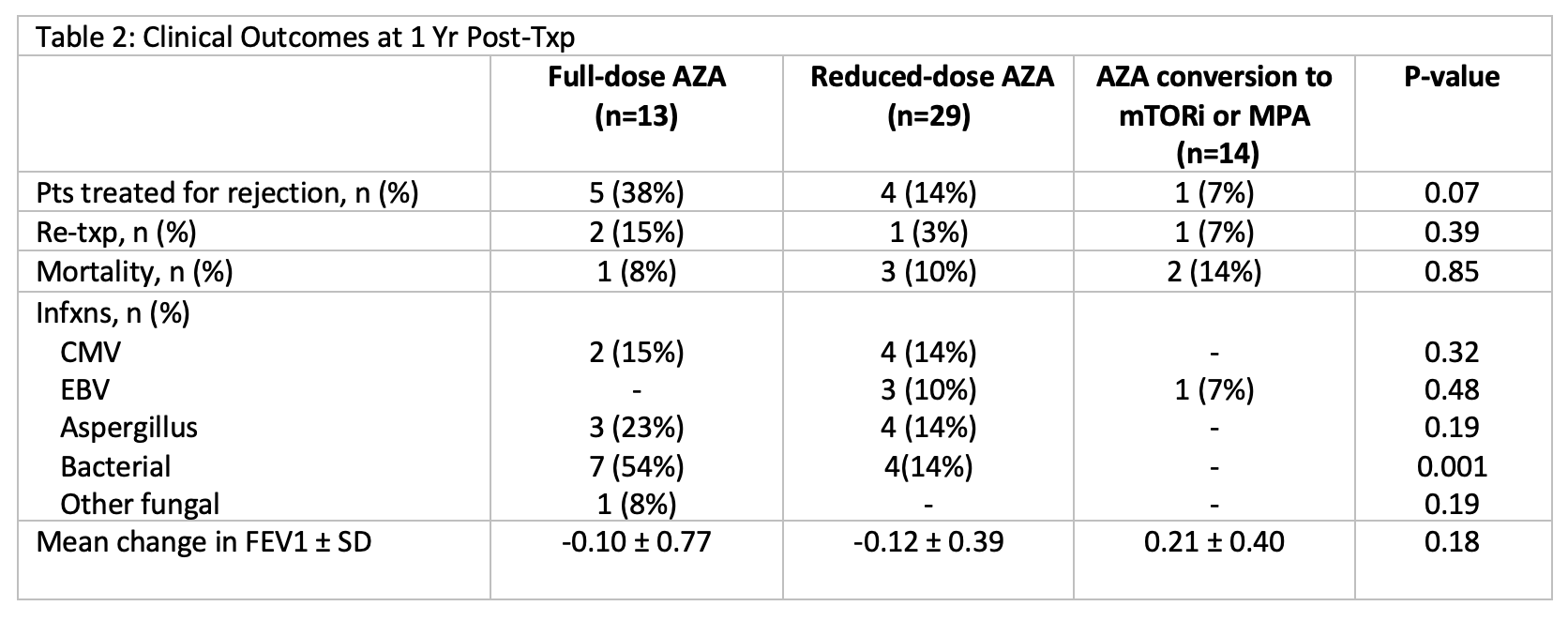
*Results: Demographics are depicted in Table 1. During the 1st yr post-txp, 29 pts (52%) required AZA reduction to a mean of 1.04 mg/kg/day, primarily due to leukopenia (69%). Fourteen pts (25%) were converted to an mTORi or MPA at a mean of 160 days post-txp. Majority of the patients who required AZA conversions (50%) were due to elevated LFTs. AZA conversion pts experienced fewer rejection episodes (7% vs 14% vs 38%; p=0.07) and fewer bacterial infxns (0% vs 14% vs 54%; p=0.001). Graft failure requiring re-txp was similar among AZA conversion and reduced-dose AZA groups but higher among full-dose AZA (7% vs 3% vs 15%; p=0.39). Mortality rates were similar across all groups (p=0.85). Both full-dose and reduced-dose AZA had similar changes in FEV1, while AZA conversion had improved FEV1 (Table 2).
*Conclusions: At 1yr post-txp, AZA treated LT pts converted to an mTORi or MPA experienced less rejection, fewer bacterial infxns, and improved FEV1 compared to full-dose and reduced-dose AZA pts. Based on these findings, a larger study should be considered to further evaluate the impact of utilizing mTORi or MPA in combination with tacrolimus in LT.
To cite this abstract in AMA style:
Chan A, Sirandas B, Carlson A, Truax C, Clark B, Hall I, Cahill B, Smith L. Is Azathioprine the Right Choice in De Novo Lung Transplantation? [abstract]. Am J Transplant. 2020; 20 (suppl 3). https://atcmeetingabstracts.com/abstract/is-azathioprine-the-right-choice-in-de-novo-lung-transplantation/. Accessed February 27, 2026.« Back to 2020 American Transplant Congress