Inhibition of TLR4 Mediated Programmed Necrosis Does Not Improve Graft Function and Histology in a Murine Kidney Transplant Model
1Renal Division, University of Colorado, Aurora, CO, 2Transplant Microsurgery Program, University of Colorado, Aurora, CO
Meeting: 2019 American Transplant Congress
Abstract number: B11
Keywords: Kidney transplantation
Session Information
Session Name: Poster Session B: Ischemia Reperfusion & Organ Rehabilition
Session Type: Poster Session
Date: Sunday, June 2, 2019
Session Time: 6:00pm-7:00pm
 Presentation Time: 6:00pm-7:00pm
Presentation Time: 6:00pm-7:00pm
Location: Hall C & D
*Purpose: Human Delayed Graft Function (DGF) is associated with upregulation of basolateral tubular TLR4 but whether TLR4 causes DGF is unknown. TLR4 has been shown to cause programmed necrosis by signaling through receptor-interacting kinases-1 and -3 (RIP-3). We observed TLR4 expression was significantly increased in WT kidneys that were subjected to CI followed by kidney transplant (CI+Txp). We hypothesized that TLR4 knockout (KO) mice would be protected from acute kidney injury (AKI) following CI+Txp.
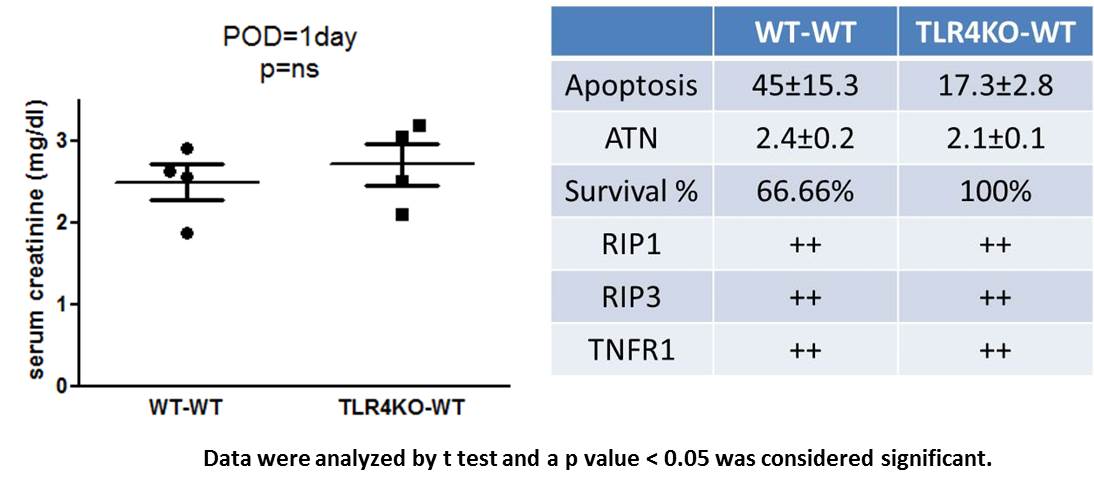
*Methods: C57Bl/6J wild type or C57Bl/6J TLR4KO kidneys were subjected to CI+Txp into wild type recipients. The recipients underwent bilateral native nephrectomy at the time of transplant. Serum creatinine (sCr) was measured 24hrs after native nephrectomy to assess transplant function. Tissue was scored for apoptosis and ATN. Protein expression was assessed by immunoblot.
*Results: Survival was significantly increased in recipients of TLR4KO kidneys (100% in TLR4KO-WT transplants vs 66.6% in WT-WT transplants, p< 0.05). However, sCr was not significantly different in recipients of WT (2.4±0.2) or TLR4KO (2.7±0.2) kidneys. RIP kinases -1, -3 were expressed after CI+Txp in both recipient groups. Tubular cell apoptosis was decreased in transplanted TLR4KO vs WT kidneys (17.3±2.8 vs 45±15.3) but this was not significant. ATN scores were similar in both groups and not significantly different. Since TNFR1 can also cause program necrosis, we examined its expression in transplanted WT and TLR4KO kidneys. Protein expression of TNFR1 was significantly increased in both WT and TLR4KO kidneys after CI+Txp.
*Conclusions: Like human DGF, we observed an increase in TLR4 expression in WT kidneys that were subjected to CI followed by kidney transplant. Survival of TLR4KO transplants was significantly improved over WT transplants and there was a trend towards decreased apoptosis. However, we observed no difference in renal function or ATN. In both WT and TLR4 KO kidneys RIP kinase 1, -3 expression was upregulated in association with increased TNFR1 expression, suggesting continued activation of programmed necrosis despite TLR4 deletion. Our results therefore suggest that multiple, possibly redundant pathways exist to trigger programmed necrosis. Deletion of TLR4 alone is insufficient to prevent renal injury, apoptosis and necrosis in kidneys subjected to CI+Txp. Our data suggest that a combined approach with inhibition of both TLR4 and TNFR1 will be needed to prevent ATN and AKI after kidney transplant.
To cite this abstract in AMA style:
Jain S, Plenter R, Nydam T, Jani A. Inhibition of TLR4 Mediated Programmed Necrosis Does Not Improve Graft Function and Histology in a Murine Kidney Transplant Model [abstract]. Am J Transplant. 2019; 19 (suppl 3). https://atcmeetingabstracts.com/abstract/inhibition-of-tlr4-mediated-programmed-necrosis-does-not-improve-graft-function-and-histology-in-a-murine-kidney-transplant-model/. Accessed March 5, 2026.« Back to 2019 American Transplant Congress