Increasing HLA DR Mismatches Is Associated with Inferior Kidney Allograft Outcome in Low Immune Risk Living Donor Kidney Transplant Recipients
Department of Medicine, Division of Nephrology, Toronto General Hospital, University of Toronto, Toronto, ON, Canada
Department of Laboratory Medicine and Pathobiology, Toronto General Hospital, University of Toronto, Toronto, ON, Canada
Meeting: 2013 American Transplant Congress
Abstract number: C1317
Background: HLA DR mismatches (MM) have been shown to negatively influence kidney allograft outcomes in historical cohorts. We examined whether this effect persists in the modern era of kidney transplantation in low immune risk living donor kidney transplant recipients.
Methods: Recipients of first, living donor, low immune risk (peak and current PRA = 0%) kidney transplant recipients (KTR) from 1 Jan 2000 to 1 Mar 2010 (follow up to 1 Mar 2011) in the Scientific Registry of Transplant Recipients were included in the study cohort. The exposure was assigned as 0, 1, or 2 HLA DR MM. Time to total graft failure (graft loss or death), death-censored graft failure, and death with graft function between groups were compared using the Kaplan-Meier method. Multivariable Cox proportional hazards models were fitted to examine the relationship between the degree of HLA DR MM and time-to-event outcomes.
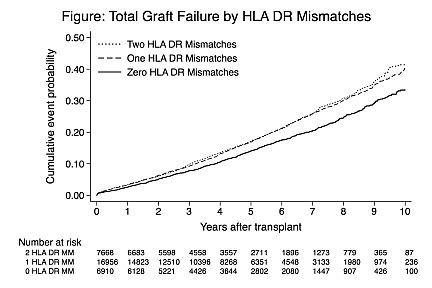
Results: A total of 31,534 patients were included in the study cohort (6,910 with 0 HLA DR MM; 16,956 with 1 HLA DR MM; 7,668 with 2 HLA DR MM). KTR with 0 HLA DR MM had the lowest total graft failure rates when compared to 1 and 2 HLA DR mismatches (log rank P < 0.0001) (Figure). The difference between 1 and 2 HLA DR MM was not significant (log rank P = 0.47). Similar patterns were observed for death-censored graft failure and death with graft function. In a multivariable Cox model, 1 and 2 HLA DR MM (vs. 0 HLA DR MM) were associated with a significant increase in the relative hazard of total graft failure (HR 1.11 [95% CI: 1.02, 1.20] and HR 1.15 [95% CI: 1.04, 1.27], respectively). Similar findings were observed for death-censored graft failure but there was no association with death with graft function.
Conclusion: In a contemporary cohort of low immune risk, living donor KTR, HLA DR MM remains as an independent predictor of graft failure. HLA DR MM may be a relevant consideration in allocation algorithms and risk assessment in low immune risk KTR.
To cite this abstract in AMA style:
Lynch S, Tinckam K, Kim J. Increasing HLA DR Mismatches Is Associated with Inferior Kidney Allograft Outcome in Low Immune Risk Living Donor Kidney Transplant Recipients [abstract]. Am J Transplant. 2013; 13 (suppl 5). https://atcmeetingabstracts.com/abstract/increasing-hla-dr-mismatches-is-associated-with-inferior-kidney-allograft-outcome-in-low-immune-risk-living-donor-kidney-transplant-recipients/. Accessed July 2, 2025.« Back to 2013 American Transplant Congress
