Impact of Transplant Center Volume on Utilization of and Outcomes Following Donation After Circulatory Death Liver Transplantation in the United States
1Digestive Disease Institute, Cleveland Clinic Abu Dhabi, Abu Dhabi, United Arab Emirates, 2Department of Quantitative Health Sciences, Cleveland Clinic Foundation, Cleveland, OH
Meeting: 2021 American Transplant Congress
Abstract number: 182
Keywords: Allocation, Donors, non-heart-beating, Liver transplantation, Outcome
Topic: Clinical Science » Liver » Liver: MELD, Allocation and Donor Issues (DCD/ECD)
Session Information
Session Name: MELD, Allocation and Donor Issues
Session Type: Rapid Fire Oral Abstract
Date: Sunday, June 6, 2021
Session Time: 6:00pm-7:00pm
 Presentation Time: 6:05pm-6:10pm
Presentation Time: 6:05pm-6:10pm
Location: Virtual
*Purpose: Despite increased utilization of donation after circulatory death (DCD) grafts in the US, impact of center volume on DCD liver transplantation (LT) remains unclear. Our aim was to evaluate impact of center volume on utilization of DCD and outcomes.
*Methods: Utilizing SRTR we evaluated all DCD LT from 2005-2019, divided into era 1: 2005-2009; era 2: 2010-2014; era 3: 2015-2019. Centers were categorized based on average annual LT as low volume (LVC): < 30, mid volume (MVC): 30-99 and high volume (HVC): > 100. Primary outcome measures were graft and patient survival. A chi-square test was used for categorical and Student’s t-test for continuous variables. Survival comparison was performed using Kaplan-Meier method and multivariable analysis using Cox proportional hazard models.
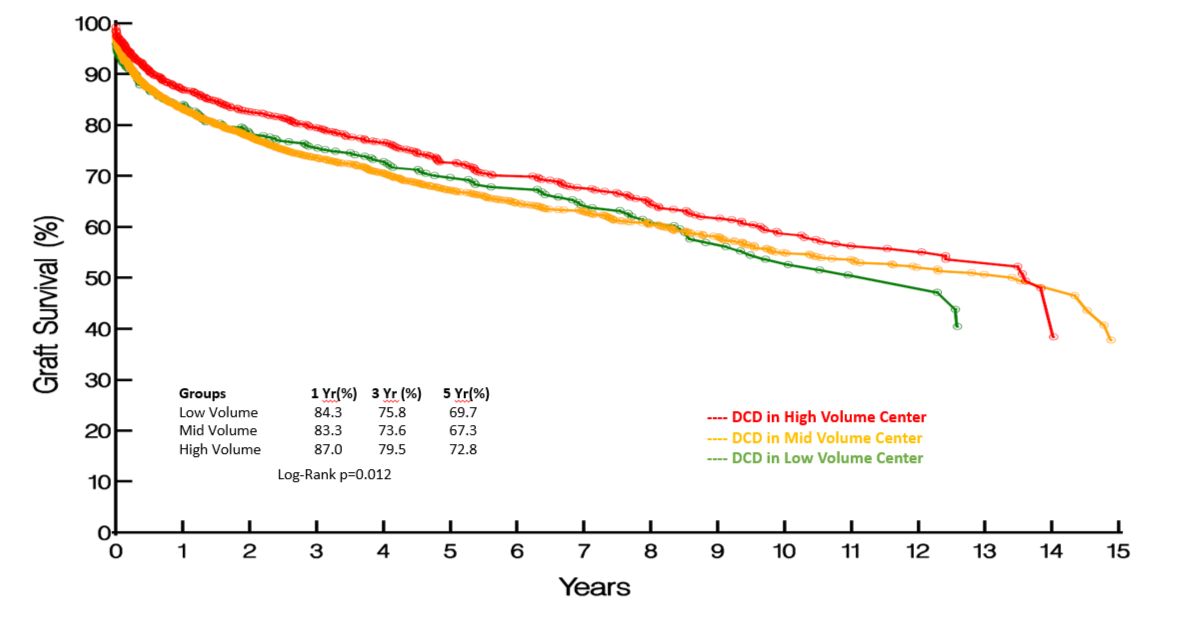
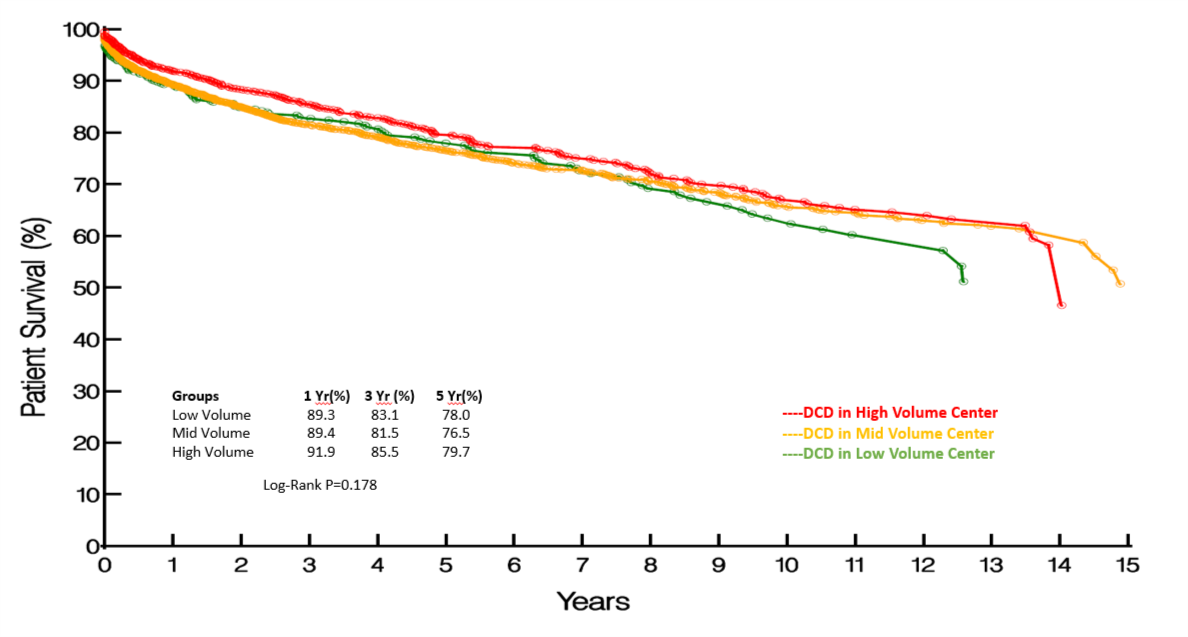
*Results: DCD LT increased from 5.2% in era 1 to 7.7% in era 3. 77% of centers used DCD donors, with the top 10 HVCs accounting for 37% of DCD LT. Proportion of DCD LT in HVC was greater in all 3 eras (%): era 1: 7.0 vs 4.8 vs 5.2; era 2: 7.1 vs 5.1 vs 4.2; era 3: 9.6 vs. 7.6 vs. 5.6 (p<0.0001). DCD recipients in HVC were more likely to be > 50 (79% vs 78% vs 72%; p=0.006) with shorter mean time from listing to LT (206 vs 277 vs 281 days; p<0.0001) and cold ischemia time (5.87 vs 6.04 vs 6.47 hours; p<0.0001). Mean donor age (37.5 vs 34.6 vs 33.7; p<0.0001) and proportion > 50 (21% vs 15% vs 13%; p<0.0001) were higher in HVC. 1-, 3- and 5-year graft survival in LVC were comparable to MVC, but inferior to HVC (Fig 1). However, 1-, 3- and 5-year patient survival were comparable in the 3 groups (Fig 2). Multivariable analysis identified recipient age, male gender, donor age, and cold ischemia time as predictors of graft and patient survival.
*Conclusions: HVCs account for a disproportionate amount of DCD LT and are more likely to transplant older recipients using older DCD donors, with shorter time from listing to LT. Expanding DCD LT in LVC and MVC may improve access and reduce waitlist mortality without compromising outcomes. Improved understanding of factors determining center variations in DCD LT will help improve organ allocation practices.
To cite this abstract in AMA style:
Kumar S, Lin S, Schold JD. Impact of Transplant Center Volume on Utilization of and Outcomes Following Donation After Circulatory Death Liver Transplantation in the United States [abstract]. Am J Transplant. 2021; 21 (suppl 3). https://atcmeetingabstracts.com/abstract/impact-of-transplant-center-volume-on-utilization-of-and-outcomes-following-donation-after-circulatory-death-liver-transplantation-in-the-united-states/. Accessed March 4, 2026.« Back to 2021 American Transplant Congress