Impact of HLA Mismatches and Cytomegalovirus Seropositivity on Outcomes Following Heart Transplantation
Division of Cardiology/ JC Walter Jr. Transplant Center, Houston Methodist Hospital, Houston, TX
Meeting: 2019 American Transplant Congress
Abstract number: B91
Keywords: Cytomeglovirus, Heart transplant patients, HLA matching
Session Information
Session Name: Poster Session B: Heart and VADs: All Topics
Session Type: Poster Session
Date: Sunday, June 2, 2019
Session Time: 6:00pm-7:00pm
 Presentation Time: 6:00pm-7:00pm
Presentation Time: 6:00pm-7:00pm
Location: Hall C & D
*Purpose: Cytomegalovirus (CMV) infection is associated with the development of cardiac allograft vasculopathy (CAV). CAV is one of the leading causes of death and graft failure beyond the first year following heart transplantation. Studies have shown a greater incidence of HLA mismatches in recipients who develop CAV than in those who do not. It is not known if presence of HLA mismatches has an additional impact on development of CAV and survival in patients with CMV seropositivity. We hypothesized that HLA mismatches leads to worse outcomes in patients with CMV seropositivity (donor or recipient related).
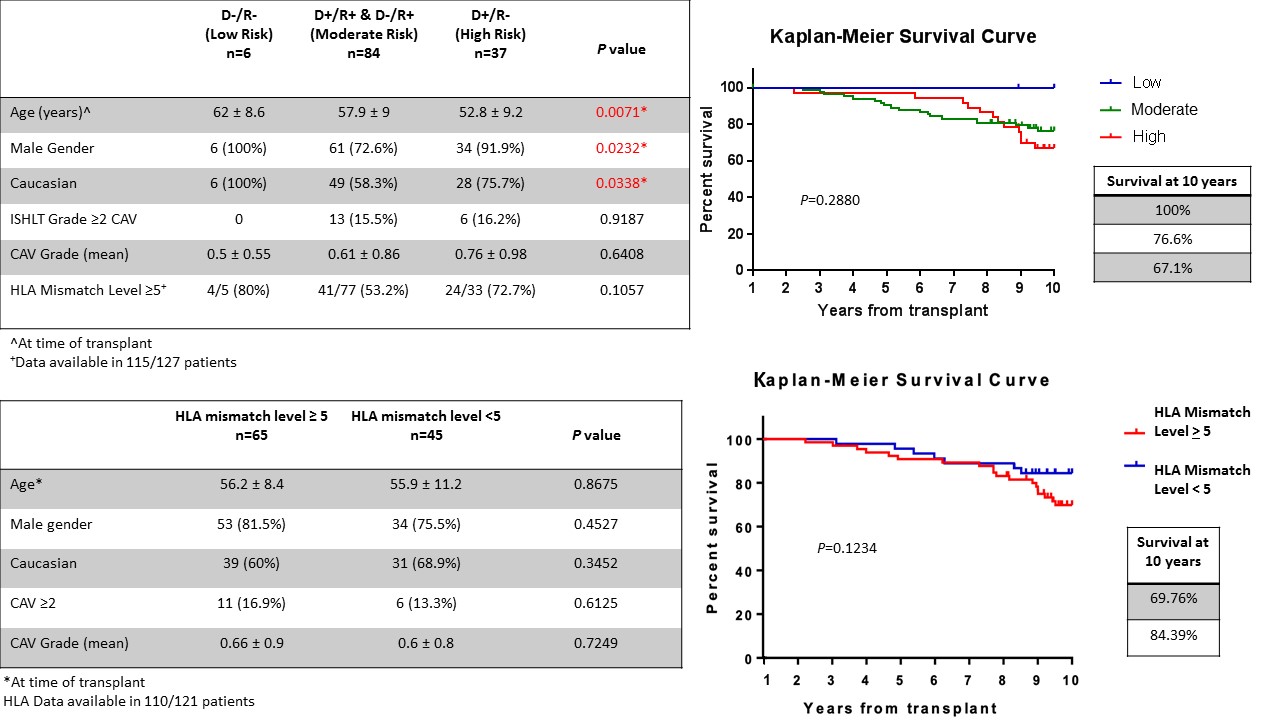
*Methods: All adult heart transplantations performed at our institution from 2000 to 2010 were retrospectively reviewed. Multi-organ transplant recipients and patients who expired within the first year after transplantation were excluded. Patients were grouped according to their CMV status: High Risk (donor positive, recipient negative), Moderate Risk (donor positive or negative, recipient positive) and Low Risk (donor and recipient negative). We analyzed development of CAV and survival. We further analyzed effect of HLA mismatch level >5 in the CMV seropositive group (Moderate and High Risk groups). Kaplan-Meier survival curves generated. P value <0.05 considered significant.
*Results: 127 heart transplant recipients were included in the analysis. CMV status was as follows: 6 (4.7%) Low Risk, 84 (66.1%) Moderate Risk and 37 (29.1%) High Risk. The least incidence of ISHLT grade > 2 CAV was in the Low Risk group, followed by Moderate Risk and greatest in the High Risk group (0% vs 15.5% vs 16.2%, P=0.92). Survival to 10 years was greatest in Low Risk, intermediate in Moderate Risk and least in the High Risk group (100% vs 76.6% vs 67.1%, P=0.29). 110 (90.9%) patients in the CMV seropositive group had HLA data available. HLA mismatch level <5 in 45 (40.9%) and >5 in 65 (59.1%). Incidence of ISHLT grade > 2 CAV was greater in patients with HLA mismatch level > 5 (16.9% vs 13.3%, P=0.61). Survival to 10 years was higher in those with HLA mismatch level <5 (84.4% vs 69.8%, P=0.12).
*Conclusions: CMV positive status (either donor or recipient) was associated with greater, but statistically insignificant, incidence of CAV and mortality. HLA mismatches in CMV positive patients was associated with a further increase, though statistically insignificant, in CAV incidence and mortality. CMV positive patients with HLA mismatches may have poorer outcomes, may need closer follow up and individualized CMV prophylaxis.
To cite this abstract in AMA style:
Singhvi A, Araujo-Gutierrez R, Park MH, Bhimaraj A, Trachtenberg BH, Hussain I, Guha A. Impact of HLA Mismatches and Cytomegalovirus Seropositivity on Outcomes Following Heart Transplantation [abstract]. Am J Transplant. 2019; 19 (suppl 3). https://atcmeetingabstracts.com/abstract/impact-of-hla-mismatches-and-cytomegalovirus-seropositivity-on-outcomes-following-heart-transplantation/. Accessed February 23, 2026.« Back to 2019 American Transplant Congress