Impact of HLA Matching on Graft Survival in Kidney Transplant Recipients
1Scientific Registry of Transplant Recipients, Minneapolis, MN, 2Department of Surgery, University of Minnesota Medical School, Minneapolis, MN, 3Department of Surgery, University of California San Francisco, San Francisco, CA
Meeting: 2022 American Transplant Congress
Abstract number: 1760
Keywords: Graft failure, HLA matching
Topic: Clinical Science » Kidney » 50 - Health Equity and Access
Session Information
Session Time: 7:00pm-8:00pm
 Presentation Time: 7:00pm-8:00pm
Presentation Time: 7:00pm-8:00pm
Location: Hynes Halls C & D
*Purpose: This study aims to estimate the association of HLA matching at the A, B, DR, and DQ loci with posttransplant graft failure and patient death among recent kidney recipients in the United States.
*Methods: Separate Cox proportional hazard models were estimated with graft failure and patient death as outcomes, respectively, for kidney-alone recipients given transplants from January 1, 2016, to December 1, 2020, and surviving at least 30 days posttransplant. The main effects of interest in these models were: a binary predictor of any or no mismatches at the A, B, and DR loci; a binary predictor of any or no mismatches at the A, B, DR, and DQ loci; categorical predictors of number of mismatches (0, 1, or 2) separately at the A, B, DR, and DQ loci. Models were adjusted for risk-adjustment covariates used in the SRTR program-specific report 3-year kidney graft survival model.
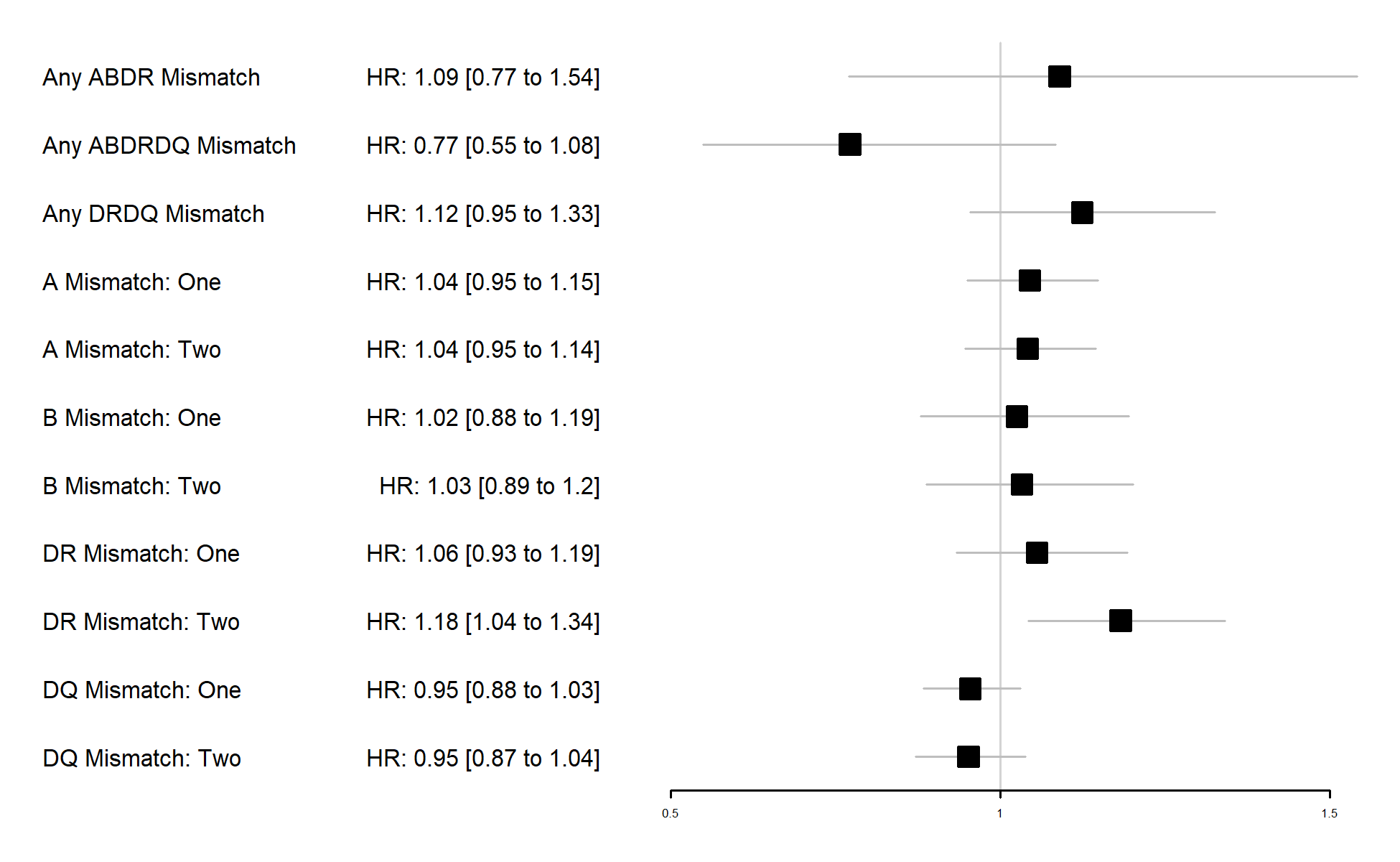
*Results: In fully adjusted models, mismatches at the DR locus were significantly associated with greater hazard for graft failure and death (Figures 1 and 2). Because DQ was hypothesized to be associated with hazard for graft failure, sensitivity analyses were conducted to describe why DQ was not associated with graft failure in fully adjusted models. In models unadjusted for mismatches at other loci, two DQ mismatches showed a significant association with graft failure. When also adjusting for DR mismatches, the DQ associations became null.
*Conclusions: Mismatches at the DR locus seem most strongly associated with the hazard of graft failure in this cohort of transplant recipients. Placing too much weight on HLA matching in organ allocation can disadvantage patients—particularly minority patients—who may have higher frequencies of HLA genotypes that are rare in donors. These analyses support matching on the DR locus in the interest of supporting kidney graft survival. Further analysis of larger cohorts with more granular outcomes may be warranted to determine the value of DQ matching. There seems to be little evidence of benefit in matching at other HLA loci based on graft survival data.
To cite this abstract in AMA style:
Miller J, Salkowski N, Thompson B, Kandaswamy R, Stock P, Israni A. Impact of HLA Matching on Graft Survival in Kidney Transplant Recipients [abstract]. Am J Transplant. 2022; 22 (suppl 3). https://atcmeetingabstracts.com/abstract/impact-of-hla-matching-on-graft-survival-in-kidney-transplant-recipients/. Accessed March 2, 2026.« Back to 2022 American Transplant Congress