Impact of Early Allograft Dysfunction (EAD) and Its Components on Patient Survival Following Liver Transplantation (LT): Long-Term Outcomes Up to 10 Years.
Transplant Division, Department of Surgery, Indiana University, Indianapolis, IN.
Meeting: 2016 American Transplant Congress
Abstract number: 444
Keywords: Liver transplantation, Outcome
Session Information
Session Name: Concurrent Session: Liver: MELD, Allocation and Donor Issues (DCD/ECD) 1
Session Type: Concurrent Session
Date: Tuesday, June 14, 2016
Session Time: 2:30pm-4:00pm
 Presentation Time: 3:18pm-3:30pm
Presentation Time: 3:18pm-3:30pm
Location: Room 304
Background: It has been shown that EAD in LT is a useful tool to predict intermediate (5-year) mortality. The purpose of this study is to determine the utility of EAD and its individual components on the prediction of long-term patient survival.
Methods: Charts from 1708 LT were reviewed between 2001-2014 at Indiana University. EAD was defined by the presence of 1 or more of the following components: (i) total bilirubin ≥10mg/dL on post-operative day (POD) 7, (ii) INR ≥1.6 on POD 7, and (iii) ALT or AST ≥2000 IU/mL within the first POD 7.
Results: Of 1708 LT, 480 (28%) had EAD. Patient survival with or without EAD was 85% or 90% at 1-year, 68% or 78% at 5-year, and 57% or 68% at 10-year. Cox-regression multivariate analysis demonstrated that EAD, MELD, donor age, recipient age, HCV, and DCD livers were significant independent variables associated with patient survival. EAD rate was higher in DCD LT (37/75, 49%). However, no survival difference was observed in DCD LT with or without EAD up to 10 years. In a cox-regression patient survival analysis controlling for MELD, donor age, and CIT; (i) if EAD defined by INR only, there was no difference in patient survival with those who did not have EAD. (ii) If EAD was defined by bilirubin only or AST/ALT only, there was a significant drop in the patient survival at 10-year (58% vs. 68%). (iii) If EAD was defined by the combination of bilirubin and AST/ALT or INR and AST/ALT, patient survival further decreased to 43% at 10-year. (iv) The worst patient survival (<20% at 10-year) was observed in EAD by the combination of INR, and bilirubin, and AST/ALT 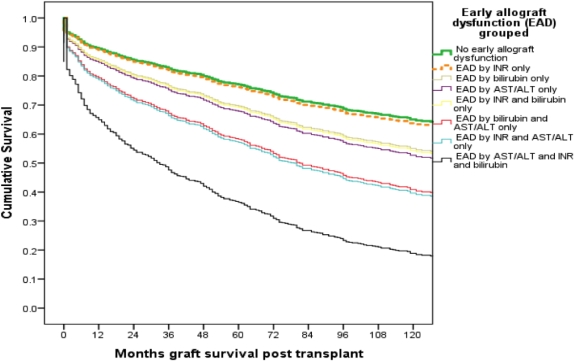 .
.
Conclusion: EAD is independently associated with decreased patient survival in the long-term in a multivariate regression model. Although EAD is more common in DCD LT, no survival disadvantage was seen compared to no-EAD DCD LT. There was incrementally worse survival at 10 years with addition of each component of EAD. EAD defined by all 3 components is associated with far worse patient survival.
CITATION INFORMATION: Ekser B, Mangus R, Fridell J, Kubal C, Davis J, Salisbury J, Salisbury T, Nagaraju S, Mihaylov P, Tector A. Impact of Early Allograft Dysfunction (EAD) and Its Components on Patient Survival Following Liver Transplantation (LT): Long-Term Outcomes Up to 10 Years. Am J Transplant. 2016;16 (suppl 3).
To cite this abstract in AMA style:
Ekser B, Mangus R, Fridell J, Kubal C, Davis J, Salisbury J, Salisbury T, Nagaraju S, Mihaylov P, Tector A. Impact of Early Allograft Dysfunction (EAD) and Its Components on Patient Survival Following Liver Transplantation (LT): Long-Term Outcomes Up to 10 Years. [abstract]. Am J Transplant. 2016; 16 (suppl 3). https://atcmeetingabstracts.com/abstract/impact-of-early-allograft-dysfunction-ead-and-its-components-on-patient-survival-following-liver-transplantation-lt-long-term-outcomes-up-to-10-years/. Accessed February 18, 2026.« Back to 2016 American Transplant Congress
