Impact of Donated Kidney Volume and Recipient Body Surface Area Incompatibility on the Allograft Outcomes with Pre-transplant Diabetes Mellitus
1Internal Medicine, Konyang University Hospital, Daejeon, Korea, Republic of, 2Internal Medicine, Seoul St. Mary's Hospital, Seoul, Korea, Republic of
Meeting: 2021 American Transplant Congress
Abstract number: 1058
Keywords: Graft survival, Kidney transplantation, Synergism
Topic: Clinical Science » Kidney » Kidney Complications: Non-Immune Mediated Late Graft Failure
Session Information
Session Name: Kidney Complications: Non-Immune Mediated Late Graft Failure
Session Type: Poster Abstract
Session Date & Time: None. Available on demand.
Location: Virtual
*Purpose: The aim of this study was to analyze the impact on the adverse allograft outcome of transplanting relative small kidneys in patients with pre-transplant diabetes mellitus (DM).
*Methods: From January 2010 to December 2018, 1,290 KTs were performed in Seoul St Mary’s Hospital. Of these, 788 cases of non-sensitized living donor kidney transplant recipient and donor pairs were enrolled. They were divided into 4 groups (non-DM large kidney, non-DM small kidney, DM large kidney, DM small kidney) according to the size incompatibility (donated kidney volume and recipient’s body surface area ratio) and pre-transplant DM status. The primary outcome of this study was to analyze the effect of size incompatibility and pre-transplant DM status on the incidence of DCGL.
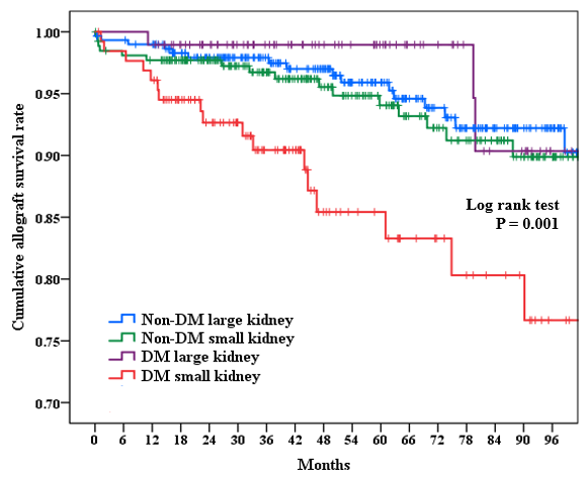
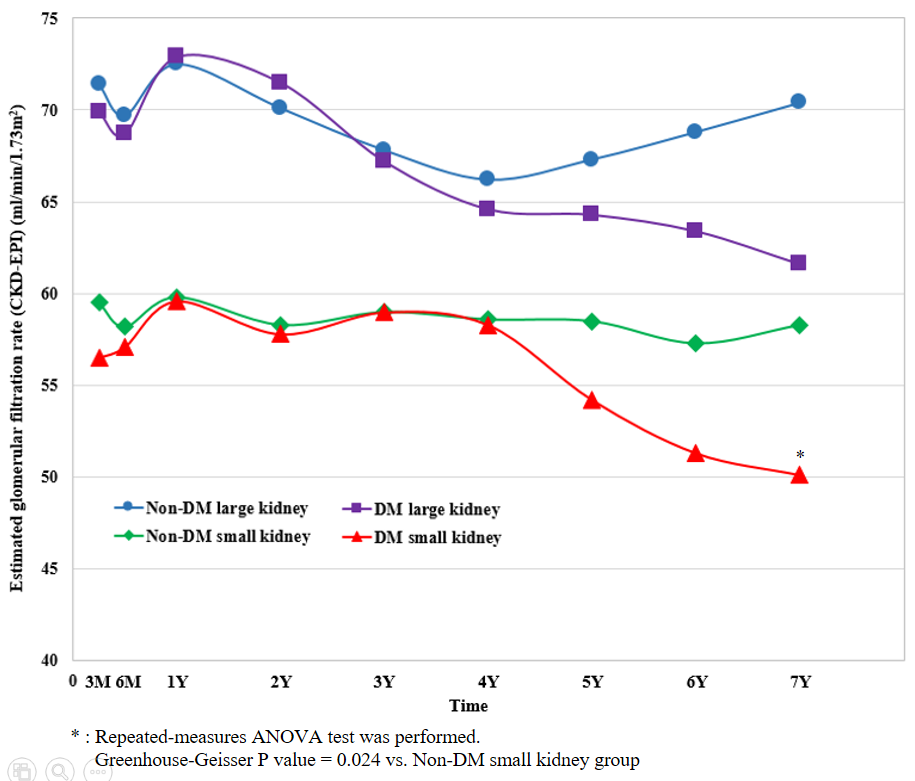
*Results: There was no significant difference in the biopsy proven acute rejection rate among the 4 groups. DM small kidney group showed significantly higher DCGL rate (17/129 (13.2%), P = 0.008) than the other groups. The combined presence of pre-transplant DM and relative small kidney was an independent risk factor for DCGL (adjusted hazard ratio 2.921, P = 0.019), and these showed significant interaction with each other (P for interaction < 0.001). Moreover, renal function after 4 years of transplantation worsened faster in the DM small kidney group compared to the other groups, and allograft survival decreased after 1 year of transplantation.
*Conclusions: Our results suggest that transplanting large kidneys rather than small kidneys is considered to have an advantage in terms of allograft outcome in pre-transplant DM patients, and this should be considered in donor selection.
| Univariable HR (95% CI) | P-value | Multivariable HR (95% CI) | P-value | P-value for interaction | |
| Pretransplant DM (-) | Reference | ||||
| Pretransplant DM (+) | 1.851 (1.057-3.243) | 0.031 | – | – | |
| Relative large kidney | Reference | ||||
| Relative small kidney | 1.908 (1.085-3.357) | 0.025 | 2.432 (1.160-5.099) | 0.019 | |
| Pretransplant DM (+) & Relative small kidney | 3.176 (1.600-6.305) | 0.001 | 2.921 (1.193-7.155) | 0.019 | <0.001 |
To cite this abstract in AMA style:
Park Y, Lee H, Ko E, Yang C, Chung B. Impact of Donated Kidney Volume and Recipient Body Surface Area Incompatibility on the Allograft Outcomes with Pre-transplant Diabetes Mellitus [abstract]. Am J Transplant. 2021; 21 (suppl 3). https://atcmeetingabstracts.com/abstract/impact-of-donated-kidney-volume-and-recipient-body-surface-area-incompatibility-on-the-allograft-outcomes-with-pre-transplant-diabetes-mellitus/. Accessed March 1, 2026.« Back to 2021 American Transplant Congress