Impact of Cold Ischemia Time on the Outcomes of Kidneys with KDPI >85%: Mate Kidney Analysis.
Nephrology, Allegheny General Hospital, Pittsburgh, PA.
Meeting: 2016 American Transplant Congress
Abstract number: 516
Keywords: Kidney transplantation
Session Information
Session Name: Concurrent Session: Kidney Waitlist Management and KAS Initial Results
Session Type: Concurrent Session
Date: Tuesday, June 14, 2016
Session Time: 4:30pm-6:00pm
 Presentation Time: 5:42pm-5:54pm
Presentation Time: 5:42pm-5:54pm
Location: Veterans Auditorium
The new kidney allocation scheme recommends simultaneous local and regional offer for kidneys with KDPI >85% in order to minimize discard rates. It is unclear whether the increase in cold ischemia time (CIT) that can come with regional sharing would adversely impact graft outcomes in these marginal kidneys.
Using OPTN/UNOS database, we identified recipients of deceased donor kidneys with KDPI >85% (calculated retrospectively) from 2000 to 2013 who were discharged on calcineurin inhibitor/mycophenolic acid based maintenance immunosuppreson. From these patients, we selected 2 groups with each group including pairs of patients who received mate kidneys from the same donor but with different CIT as follows: Group 1= CIT ≥12 but <24 hours (n=747) vs. CIT ≥24 hours (n=747); group 2= CIT <12 hours (n=127) vs. CIT ≥24 hours(n=127). Cox regression analysis adjusting for recipient and transplant related factors was used to compare delayed graft function (DGF), overall graft failure and patient death risks between mate kidneys with different CIT under each group. Recipient and transplant characteristics between mate kidney recipients in each group were similar except for the following: more frequent machine perfusion for CIT ≥24h kidneys than mate kidneys in groups 1 (65 vs. 55%, p<0.001) and 2 (58 vs. 32%, p<0.01), while PRA>30% was less frequent in transplant recipients with CIT <12h in group 2 (19 vs. 10%, p=0.03).There were no significant differences in length of stay and acute rejection at discharge between mate kidney groups. The incidence of DGF was significantly lower with a trend towards lower graft failure risk for patients with CIT <12h in group 2 (Table 1, figure 1).
| Delayed graft function | Adjusted graft failure risk | Adjusted patient death risk | ||||
| OR | 95% CI | HR | 95% CI | HR | 95% CI | |
| Group 1: (CIT ≥12h but <24h vs. CIT ≥24 h) | 0.82 | 0.65-1.03 | 0.93 | 0.77-1.13 | 0.83 | 0.65-1.05 |
| Group 2: (CIT <12h vs. CIT ≥24h) | 0.38* | 0.21-0.66 | 0.68** | 0.43-1.08 | 0.98 | 0.55-1.73 |
| p-value: * = <0.001, ** = 0.11 | ||||||
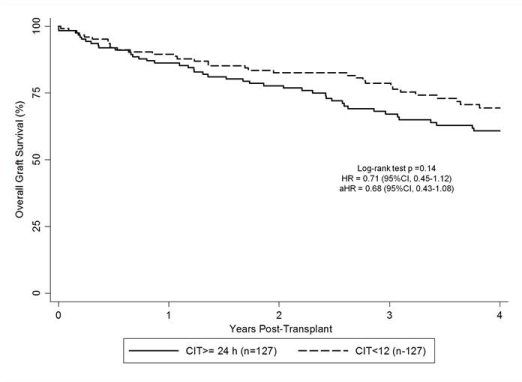
Our findings strongly favor keeping CIT <12 hours in deceased donor kidneys with KDPI [rsaquo]85% in order to optimize outcomes of regional sharing of these organs.
CITATION INFORMATION: Sampaio M, Chopra B, Sureshkumar K. Impact of Cold Ischemia Time on the Outcomes of Kidneys with KDPI >85%: Mate Kidney Analysis. Am J Transplant. 2016;16 (suppl 3).
To cite this abstract in AMA style:
Sampaio M, Chopra B, Sureshkumar K. Impact of Cold Ischemia Time on the Outcomes of Kidneys with KDPI >85%: Mate Kidney Analysis. [abstract]. Am J Transplant. 2016; 16 (suppl 3). https://atcmeetingabstracts.com/abstract/impact-of-cold-ischemia-time-on-the-outcomes-of-kidneys-with-kdpi-85-mate-kidney-analysis/. Accessed July 12, 2025.« Back to 2016 American Transplant Congress
