Impact of Aortic Abdominal Calcification among Living Donor Liver Transplant Recipients; a Retrospective Study
Gastroenterological and Transplant Surgery, Hiroshima University, Hiroshima, Japan.
Meeting: 2018 American Transplant Congress
Abstract number: C232
Keywords: Liver transplantation, Outcome
Session Information
Session Name: Poster Session C: Liver: Recipient Selection
Session Type: Poster Session
Date: Monday, June 4, 2018
Session Time: 6:00pm-7:00pm
 Presentation Time: 6:00pm-7:00pm
Presentation Time: 6:00pm-7:00pm
Location: Hall 4EF
Abdominal aortic calcification (AAC) is known as a risk factor of coronary artery disease, stroke, hyperphosphatemia, chronic inflammation, diabetes, and decreased an estimated glomerular filtration rate. We analyzed the outcomes of living donor liver transplantation (LDLT) for patients with AAC. Of 141 consecutive patients with LDLT between January 2007 and December 2014, we divided the patients into two groups according to the AAC levels calculated by AZE Virtual Place Lexus64 Anatomia software. The survival time of patients with low AAC was significantly longer than that of patients with high AAC (median survival time 5.08 vs 2.95 years [p = 0.0101]) even after propensity score matching. 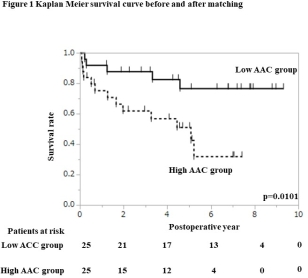 Multivariate analysis identified the high AAC (hazard ratio 2.167) and old donor (hazard ratio 2.291) as prognostic factors for overall survival.
Multivariate analysis identified the high AAC (hazard ratio 2.167) and old donor (hazard ratio 2.291) as prognostic factors for overall survival.
| Multivariate analysis | OR | CI | p-value |
| Donor age (Y) ≥50 | 2.2910 | 1.2158-4.1585 | 0.0114 |
| AAC (mm3) ≥100 | 2.1667 | 1.2087-3.9425 | 0.0095 |
There was no effect of high AAC on post-operative complications. However, high AAC leads to worse survival in patients with blood stream infection after LDLT (p = 0.0313). 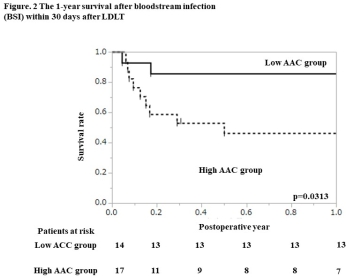 In conclusion, high AAC was an independent unfavorable prognostic factor.
In conclusion, high AAC was an independent unfavorable prognostic factor.
CITATION INFORMATION: Imaoka Y., Ohira M., Simizu S., Tahara H., Ide K., Tanaka Y., Ohdan H. Impact of Aortic Abdominal Calcification among Living Donor Liver Transplant Recipients; a Retrospective Study Am J Transplant. 2017;17 (suppl 3).
To cite this abstract in AMA style:
Imaoka Y, Ohira M, Simizu S, Tahara H, Ide K, Tanaka Y, Ohdan H. Impact of Aortic Abdominal Calcification among Living Donor Liver Transplant Recipients; a Retrospective Study [abstract]. https://atcmeetingabstracts.com/abstract/impact-of-aortic-abdominal-calcification-among-living-donor-liver-transplant-recipients-a-retrospective-study/. Accessed February 22, 2026.« Back to 2018 American Transplant Congress
