Impact of Antecedent Malignancy on Kidney Transplant Outcomes: Patient, Graft, and Cancer-Free Survival
1Surgery, University of Minnesota, Minneapolis, MN
2Biostatistical Design and Analysis Center, Clinical and Translational Science Institute, Minneapolis, MN
3Biostatistics, University of Minnesota, Minneapolis, MN.
Meeting: 2018 American Transplant Congress
Abstract number: B348
Keywords: Kidney transplantation, Malignancy, Recurrence, Survival
Session Information
Session Name: Poster Session B: PTLD/Malignancies: All Topics
Session Type: Poster Session
Date: Sunday, June 3, 2018
Session Time: 6:00pm-7:00pm
 Presentation Time: 6:00pm-7:00pm
Presentation Time: 6:00pm-7:00pm
Location: Hall 4EF
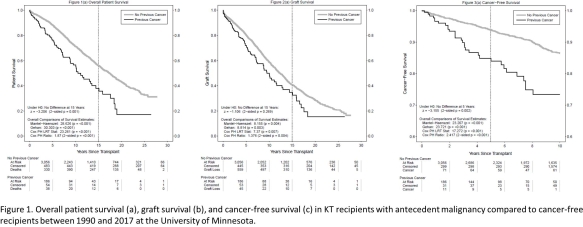
OBJECTIVE: Non-skin pretransplant malignancy (NSPTM) has historically been considered a relative contraindication to kidney transplantation (KT). In addition to the conventional risk factors for cancer, KT recipients have the additive immunosuppression risk, which can have an impact on the development of post-transplant malignancy (PoTM). We sought to assess the impact of NSPTM on patient, graft, and cancer-free survival after KT.
METHODS: Between 1990 and 2017, we performed 3242 KT at our institution; 186 (5.7%) had NSPTM. The incidence and type of malignancy in the NSPTM cohort was analyzed. Posttransplant patient, graft, and cancer-free survival were compared and the relative risk of developing a PoTM was calculated.
RESULTS: Of the 186 KT recipients in the NSPTM group, prostate (26.3%), kidney (18.8%), and colon (8.6%) cancer were most prevalent. After a median follow-up of 10.2 years in the control group and 6.6 years in the NSPTM group, 477 (15.6%) and 35 (18.8%) recipients developed PoTM, respectively. The most common PoTM in the control group were lymphoma (23.1%), melanoma (13.0%), and kidney cancer (10.3%); and melanoma (5.7%) in the NSPTM group. When compared to the control group, the NSPTM cohort exhibited lower patient (Fig. 1a; p=0.001) and cancer-free (1c; p=0.002) survival but not graft survival (1b; p=0.269). On multivariate analysis, NSPTM was associated with decreased patient (hazard ratio 1.63; 95% confidence interval 1.20-2.21) and graft (1.39; 1.06-1.83) survival but not incidence PoTM (1.39; 0.91-2.13). The most common cause of death in the control group was cardiovascular disease (21.2%); whereas malignancy was the most common cause of death in the NSPTM group (23.7%).
CONCLUSION: KT recipients with an antecedent malignancy exhibit lower posttransplant patient survival and higher graft loss but an equivalent incidence of PoTM.
CITATION INFORMATION: Serrano O., Mongin S., Berglund D., Vock D., Chinnakotla S., Dunn T., Finger E., Kandaswamy R., Pruett T., Matas A. Impact of Antecedent Malignancy on Kidney Transplant Outcomes: Patient, Graft, and Cancer-Free Survival Am J Transplant. 2017;17 (suppl 3).
To cite this abstract in AMA style:
Serrano O, Mongin S, Berglund D, Vock D, Chinnakotla S, Dunn T, Finger E, Kandaswamy R, Pruett T, Matas A. Impact of Antecedent Malignancy on Kidney Transplant Outcomes: Patient, Graft, and Cancer-Free Survival [abstract]. https://atcmeetingabstracts.com/abstract/impact-of-antecedent-malignancy-on-kidney-transplant-outcomes-patient-graft-and-cancer-free-survival/. Accessed February 18, 2026.« Back to 2018 American Transplant Congress