Immunologic Long-Term Outcome of Living Kidney Transplantation Depending On the Donor-Recipient Relationship
D. Khadzhynov, F. Halleck, D. Schmidt, S. Kreimer, K. Budde, O. Staeck.
Nephrology, Charite Universitaetsmedizin Berlin, Berlin, Germany.
Meeting: 2015 American Transplant Congress
Abstract number: B170
Keywords: Donors, Graft survival, Kidney transplantation, Outcome, unrelated
Session Information
Session Name: Poster Session B: Living Donor Issues 1
Session Type: Poster Session
Date: Sunday, May 3, 2015
Session Time: 5:30pm-6:30pm
 Presentation Time: 5:30pm-6:30pm
Presentation Time: 5:30pm-6:30pm
Location: Exhibit Hall E
Background. Only few data is available about long-term immunologic outcomes of living kidney transplantation (KTx) depending on the donor-recepient relationship.
Patients and methods. This single center retrospective long-term observational study included related (parent-to-child or siblings) and unrelated adult living donor kidney transplant recipients between 2000 and 2014 (n=335) (Table 1). DSA analysis and allograft biopsies were performed for clinically suspected rejections. Data analysis included patient and graft survival, biopsy proven rejection episodes (T-cell mediated (TCMR) or antibody mediated (ABMR)) and development of de-novo DSA. Outcome data were assessed over a period of maximum 14 years.
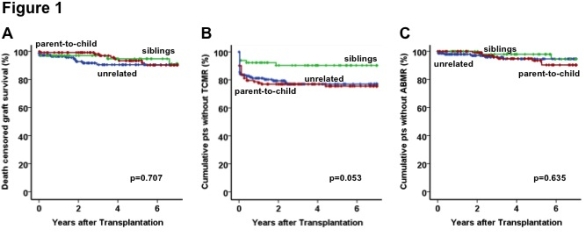
Results. Graft survival did not differ significantly among the groups (Fig 1A). Sibling-to-sibling pares trend to result in a lower incidence of TCMR (Fig 1-B). There was no significant difference between the groups in terms of ABMR (Fig 1-C). The rates of de novo DSA tended to be higher in parent-to-child pares and non-related KTx (both 26% after 7 years vs. 11% in siblings, p=0.102). The multivariate analysis adjusted for age, AB0-incompatibility, HLA (A, B, DR)-mismatch and donor-recipient relationship identified the donation by a sibling as an independent protective factor for TCMR (HR 0.347, p=0.018). The number of HLA-mismatches was shown to be the only independent risk factor for de-novo DSA (HR 1.21, p=0.012).
Conclusion. Not only HLA-mismatch but also donor-recepient relationship does influence the immunological outcome significantly. Our data suggest donation by a sibling is an independent protective factor for TCMR.
| Patient characteristics | Not related living KTx, n=146 | Sibling-to-sibling, n=66 | Parent-to-child, n=123 | P-value |
| Mean recipient age, years (SD) | 53 (10) | 45 (11) | 30 (8) | <0.001 |
| Mean donor age, years (SD) | 51 (10) | 43 (12) | 54 (8) | <0.001 |
| Recipient male, n | 103 (71%) | 41 (62%) | 81 (66%) | 0.445 |
| Donor male, n | 46 (32%) | 32 (49%) | 41 (33%) | 0.052 |
| Prior kidney transplantation, n | 7 (5%) | 7 (11%) | 4 (3%) | 0.113 |
| AB0 incompatible, n | 18 (12%) | 1 (1.5%) | 10 (8%) | 0.024 |
| Mean HLA-mismatches (SD) | 4.1 (1.2) | 1.9 (1.5) | 2.1 (0.9) | <0.001 |
To cite this abstract in AMA style:
Khadzhynov D, Halleck F, Schmidt D, Kreimer S, Budde K, Staeck O. Immunologic Long-Term Outcome of Living Kidney Transplantation Depending On the Donor-Recipient Relationship [abstract]. Am J Transplant. 2015; 15 (suppl 3). https://atcmeetingabstracts.com/abstract/immunologic-long-term-outcome-of-living-kidney-transplantation-depending-on-the-donor-recipient-relationship/. Accessed March 7, 2026.« Back to 2015 American Transplant Congress
