Identification Of Pre-transplant Biomarkers Of Recipient Immune Dysfunction That Predict Recipient Risk Of Death Following Liver Transplant: The Immune Frailty Index
1Sherrie and Alan Conover Center for Liver Disease and Transplantation, Houston Methodist Hospital, Houston, TX, 2Department of Pathology and Genomic Medicine, Houston Methodist Hospital, Houston, TX
Meeting: 2019 American Transplant Congress
Abstract number: 469
Keywords: High-risk, Liver transplantation, Mortality, Survival
Session Information
Session Name: Concurrent Session: Biomarkers, Immune Monitoring and Outcomes IV
Session Type: Concurrent Session
Date: Tuesday, June 4, 2019
Session Time: 2:30pm-4:00pm
 Presentation Time: 3:06pm-3:18pm
Presentation Time: 3:06pm-3:18pm
Location: Room 306
*Purpose: Cirrhosis-related immune dysfunction is well recognized and likely contributes to early mortality following liver transplant (LT) resulting from infections; however, few prior studies have evaluated predictors of critical pre-transplant immune dysfunction which might forecast early mortality after liver transplant. The present study evaluates a panel of pre-transplant immunologic biomarkers predictive of post-LT mortality.
*Methods: From 2013-17, plasma from 125 LT recipients was analyzed day -1 relative to LT via Luminex (Biorad) compared to normal healthy controls (n=17). Recipient clinical data was correlated with a pre-selected panel of chemokines/cytokines (sIL6rB, GCP-2, CCL1, SDF, MMP2, TNFa, BAFF, Eotaxin, MMP3, IP-10, IL-10, CTACK, and Fractalkine).
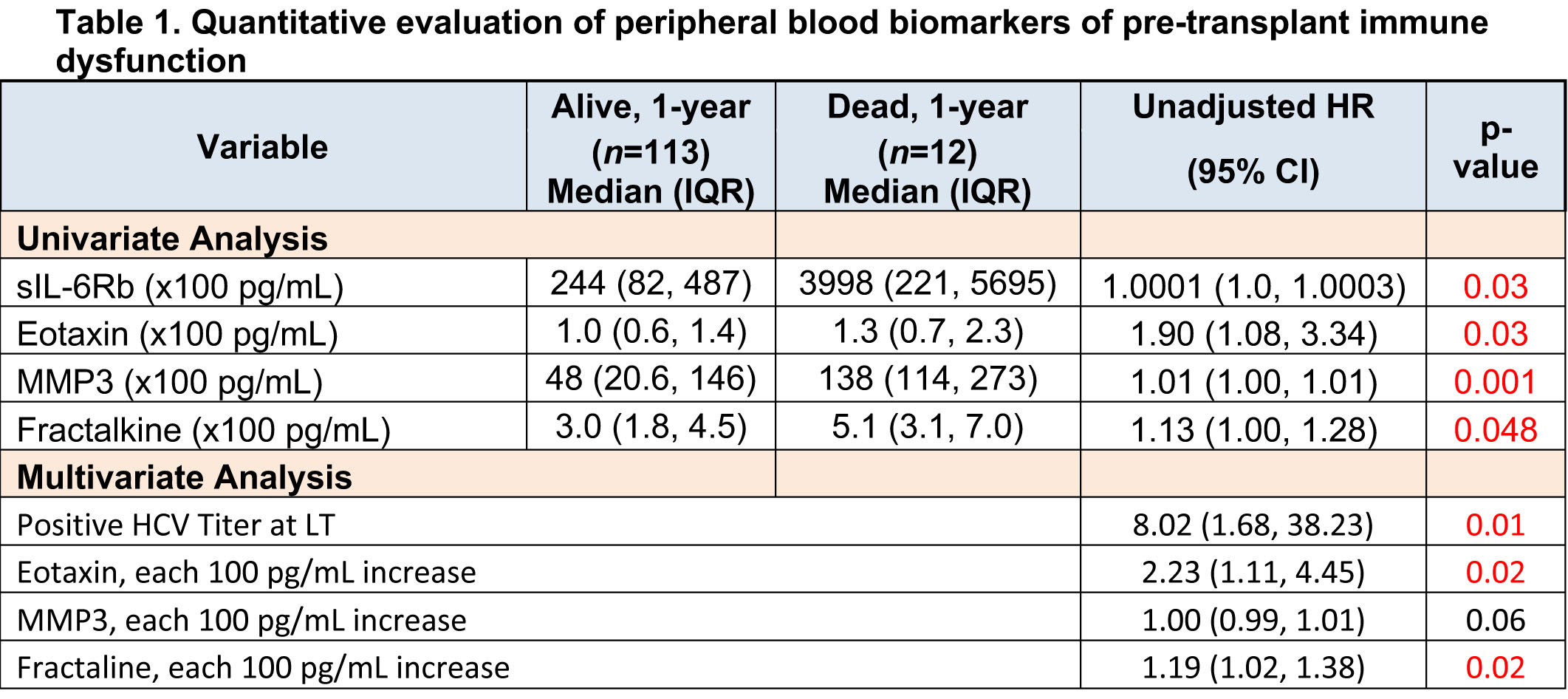
*Results: Of assayed chemokines and cytokines, all but GCP-2 (p=0.09) were significantly elevated prior to LT compared to normal controls (p<0.01). One-yr pt survival was 90.4%. Correlation with mortality was assessed with univariate Cox Proportional Hazard modeling. Median MELD was 31 for pts alive at 1yr vs. 33 for pts who died (p=0.7). Among demographics, alcoholic liver disease (HR 0.1, p=0.03) and detectable HCV viral load (HR 4.93, p=0.01) correlated with survival. Pts who died had similar medical acuity to pts alive >1yr but were more likely to have pre-LT SBP (p<0.001). Eotaxin, MMP3, Fractalkine, and sIL6Rb all positively correlated with 1-yr mortality (Table 1).
On multivariate modeling, HCV, Eotaxin, MMP3, and Fractalkine predicted 1yr mortality (C-statistic=0.84). An immune frailty index (IFI) was then created by assigning 1 point for each predictive factor for values exceeding the median threshold. Patients with a low IFI (Score 0-2) had 95.5% 1yr survival compared with 46.2% for patients with high IFI (Score 3-4) (Figure 1).
*Conclusions: We have identified pre-transplant Eotaxin, Fractalkine, and MMP3 as potential biomarkers to predict post-transplant mortality. The resulting IFI has potential to identify patients at increased risk for futile outcomes prior to LT and augment clinical assessment among high acuity recipients. These data provide initial insight into the immune dysfunction in cirrhotic recipient affecting post-LT outcomes.
To cite this abstract in AMA style:
Lunsford KE, Aware N, Cleveland K, Manner CJ, Nguyen DT, Graviss EA, Thomas JV, Vyas H, Moore LW, Dorman SA, Saharia A, Mobley CM, Hobeika MJ, Li XC, Ghobrial RM. Identification Of Pre-transplant Biomarkers Of Recipient Immune Dysfunction That Predict Recipient Risk Of Death Following Liver Transplant: The Immune Frailty Index [abstract]. Am J Transplant. 2019; 19 (suppl 3). https://atcmeetingabstracts.com/abstract/identification-of-pre-transplant-biomarkers-of-recipient-immune-dysfunction-that-predict-recipient-risk-of-death-following-liver-transplant-the-immune-frailty-index/. Accessed February 22, 2026.« Back to 2019 American Transplant Congress