Hypernatremia Predicts Waitlist Death and Deterioration, but Not Post-Transplant Outcomes in Pediatric Liver Transplant Candidates
1Anesthesiology, Mayo Clinic, Rochester, MN, 2Surgery, Mayo Clinic, Rochester, MN, 3Pediatric Gastroenterology, Mayo Clinic, Rochester, MN, 4Gastroenterology, Mayo Clinic, Rochester, MN
Meeting: 2020 American Transplant Congress
Abstract number: D-141
Keywords: Allocation, Liver transplantation, Outcome, Pediatric
Session Information
Session Name: Poster Session D: Liver: Pediatrics
Session Type: Poster Session
Date: Saturday, May 30, 2020
Session Time: 3:15pm-4:00pm
 Presentation Time: 3:30pm-4:00pm
Presentation Time: 3:30pm-4:00pm
Location: Virtual
*Purpose: Pre-transplant hypernatremia has been shown to predict post-transplant mortality in adult liver transplant (LT) recipients. The effects of hypernatremia in children, however, remain unexplored. We sought to delineate the impact of hypernatremia on both waitlist, and post-transplant outcomes in pediatric LT patients.
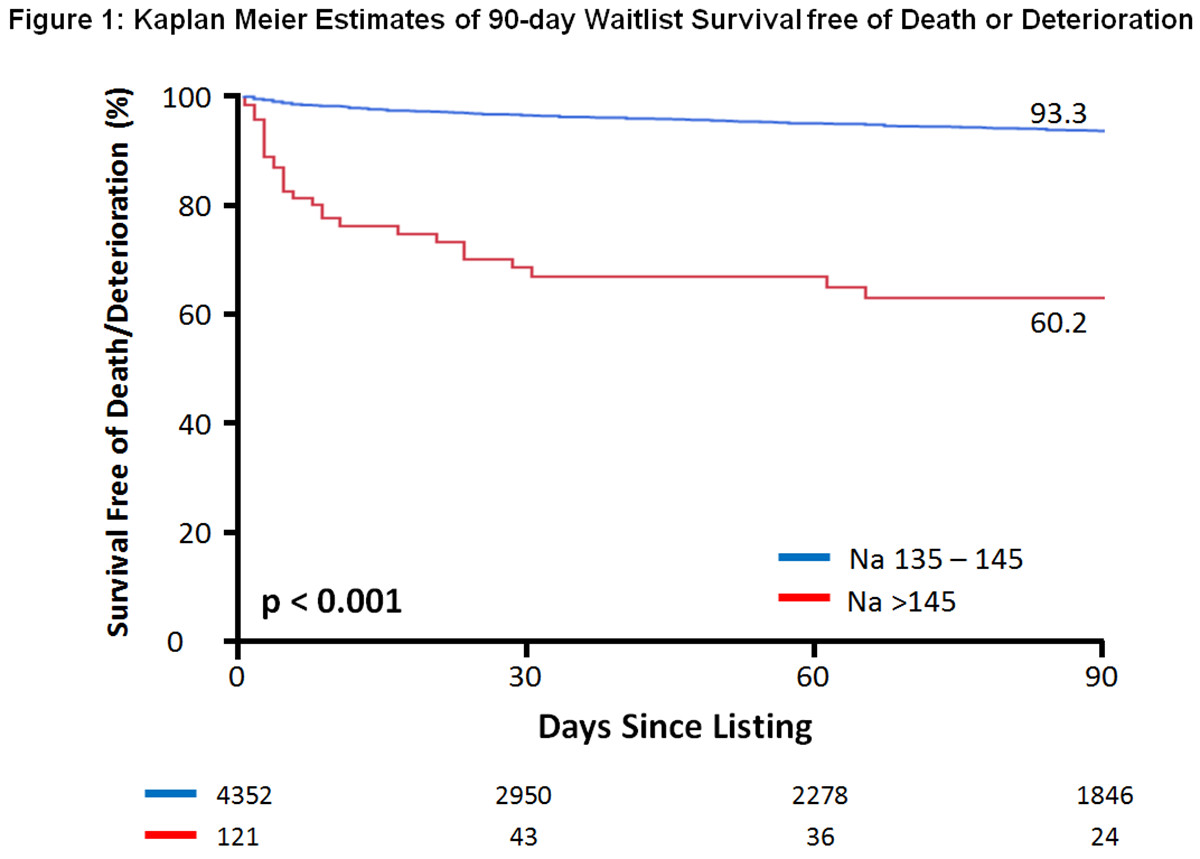
*Methods: We studied all pediatric patients (<12-years) listed for isolated LT in the United States between February 2002 - June 2018. The relationship between serum sodium and both 90-day waitlist death/deterioration, and 90-day post-transplant survival were analyzed using Kaplan Meier methods and Cox proportional-hazards models.
*Results: Serum sodium at wait-listing was available for 5,435/6,522 (83%) patients. Hypernatremia (>145mEq/L) was found in 121 (2.2%), versus 4,352 (80.1%) with normonatremia (135-145mmol/L). Compared with normonatremia, hypernatremic patients were sicker, as demonstrated by higher listing Pediatric End-Stage Liver Disease (PELD) scores (median 17 [IQR 8-25] vs 8 [-3-20], p<0.001), and lower glomerular filtration rates (eGFR) (median [IQR] 89ml/min/1.73cm2 [53-124] vs 129ml/min/1.73cm2 [99 – 160], p<0.001). Estimates of 90-day waitlist survival free of death/deterioration were significantly inferior in hypernatremic patients (Figure 1). When accounting for the confounding effects of PELD and renal function, hypernatremia independently predicted a 3-fold increase in the risk of 90-day waitlist death/deterioration (HR 3.12, 95%CI 2.07-4.71; p<0.001). In patients with hypernatremia at time of transplant, unadjusted estimates of 90-day post-transplant survival were 93.4%, versus 96.8% in normonatremic patients (p=0.005). After adjusting for PELD, renal function, cold ischemia time and whole vs. split-graft type, hypernatremia did not confer an added risk of 90-day post-transplant mortality (HR 1.51, 95%CI 0.88-2.57; p=0.135).
*Conclusions: Hypernatremia is rare in pediatric LT candidates, but is frequently associated with more severe disease. While hypernatremia independently predicts inferior 90-day waitlist outcomes, patients that successfully proceed to transplantation do not appear to be disadvantaged with regards to post-transplant survival. As such, consideration should be given for the inclusion of serum sodium in risk stratification models for pediatric liver transplant allocation.
To cite this abstract in AMA style:
Thalji L, Thalji N, Ibrahim S, Heimbach J, Kamath P, Haile D, Kor D. Hypernatremia Predicts Waitlist Death and Deterioration, but Not Post-Transplant Outcomes in Pediatric Liver Transplant Candidates [abstract]. Am J Transplant. 2020; 20 (suppl 3). https://atcmeetingabstracts.com/abstract/hypernatremia-predicts-waitlist-death-and-deterioration-but-not-post-transplant-outcomes-in-pediatric-liver-transplant-candidates/. Accessed March 7, 2026.« Back to 2020 American Transplant Congress