Hospitalizations for Cardiovascular Disease After Liver Transplantation in the United States: Epidemiology, Outcomes, and Costs.
Transplant Center, Mayo Clinic, Phoenix.
Meeting: 2016 American Transplant Congress
Abstract number: 327
Keywords: Liver transplantation, Mortality, Multivariate analysis, Outcome
Session Information
Session Name: Concurrent Session: Liver Transplantation Peri-Operative Considerations
Session Type: Concurrent Session
Date: Monday, June 13, 2016
Session Time: 4:30pm-6:00pm
 Presentation Time: 4:54pm-5:06pm
Presentation Time: 4:54pm-5:06pm
Location: Room 311
Background: Cardiovascular disease (CVD) is a leading cause of post-liver transplant death, and variable care patterns may affect outcomes. We aimed to describe epidemiology, outcomes, and costs of inpatient CVD care across U.S. hospitals.
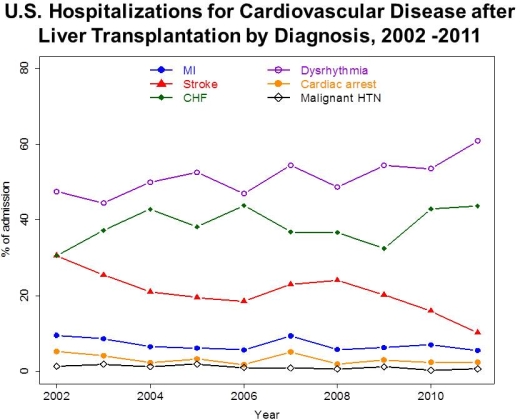
Methods: Using a merged dataset from the 2002-2011 Nationwide Inpatient Sample and the American Hospital Association Annual Survey, we evaluated liver transplant patients admitted primarily with myocardial infarction (MI), stroke (CVA), CHF, dysrhythmias, cardiac arrest (CA), or malignant hypertension. Patient-level data include demographics, APR-DRG co-morbidity burden, and CVD diagnoses. Facility level variables included ownership status, payer-mix, hospital resources, teaching status, and physician/nursing-to-bed ratios. Cost quartiles were based on facility-specific cost-charge ratios. We used generalized estimating equations to evaluate patient and hospital-level factors associated with mortality and costs.
Results: 4,763 hospitalizations occurred in 153 facilities (Transplant hospitals n=80). CVD hospitalizations increased overall by 115% over the decade (p<0.01). CVA and MI declined over time (both, p<0.05), but CHF and dysrhythmia grew significantly (both, p<0.03), as shown below. 19% hospitalizations were for multiple CVD diagnoses. Transplant hospitals had lower co-morbidity patients (p<0.001),and had greater resource intensity including presence of cardiac ICU, interventional radiology, operating rooms, teaching status, and nursing density (all, p<0.01). CA and MI were associated with the highest mortality rates (p<0.001). Transplant and non-transplant hospitals had similar mortality (overall, 3.9%, p=0.55). High CVD burden (aOR 3.35, p <0.001), emergent admission (aOR 1.50, p=0.06), and high expense hospitals (aOR 1.70, p=0.03) predicted mortality. High cost was associated with high CVD burden (aOR 2.11, p=0.001).
Conclusions: CVD after liver transplant is evolving and responsible for growing rates of inpatient care. High CVD burden predicted mortality and high cost care, which should direct QI efforts.
CITATION INFORMATION: Mathur A, Chang Y.-H, Steidley D, Khurmi N, Katariya N, Singer A, Hewitt W, Reddy K, Moss A. Hospitalizations for Cardiovascular Disease After Liver Transplantation in the United States: Epidemiology, Outcomes, and Costs. Am J Transplant. 2016;16 (suppl 3).
To cite this abstract in AMA style:
Mathur A, Chang Y-H, Steidley D, Khurmi N, Katariya N, Singer A, Hewitt W, Reddy K, Moss A. Hospitalizations for Cardiovascular Disease After Liver Transplantation in the United States: Epidemiology, Outcomes, and Costs. [abstract]. Am J Transplant. 2016; 16 (suppl 3). https://atcmeetingabstracts.com/abstract/hospitalizations-for-cardiovascular-disease-after-liver-transplantation-in-the-united-states-epidemiology-outcomes-and-costs/. Accessed February 24, 2026.« Back to 2016 American Transplant Congress
