Hospital Characteristics Mediate Variation in Cirrhosis Mortality in Transplant and Non-Transplant Facilities
1Surgery, Mayo Clinic Arizona, Phoenix, AZ
2Surgery, University of Michigan, Ann Arbor, MI
3Medicine, University of Michigan, Ann Arbor, MI.
Meeting: 2015 American Transplant Congress
Abstract number: A222
Keywords: Liver cirrhosis, Liver transplantation, Outcome, Prediction models
Session Information
Session Name: Poster Session A: Non Organ Specific, Economics, Public Policy, Allocation, Ethics
Session Type: Poster Session
Date: Saturday, May 2, 2015
Session Time: 5:30pm-7:30pm
 Presentation Time: 5:30pm-7:30pm
Presentation Time: 5:30pm-7:30pm
Location: Exhibit Hall E
Hospitals vary significantly in cirrhosis mortality. We aimed to determine whether hospital structural characteristics mediate this effect.
Methods: We used 2009 data from the HCUP Nationwide Inpatient Sample and the American Hospital Association to create a multi-level model to evaluate the effect of patient factors and specific hospital characteristics on risk of in-patient mortality from cirrhosis. Structural factors were cumulatively added to the model to determine how much a specific factor affected inter-hospital variation in cirrhosis mortality.
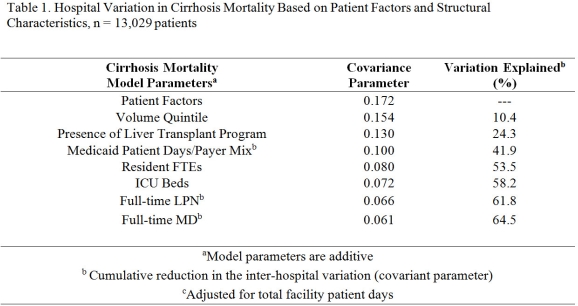
Results: 13,029 cirrhosis admissions were sampled in 477 hospitals. Patient characteristics including age, sex, race, payer status, and APR-DRG morbidity varied significantly by hospital cirrhosis volume (p < 0.05). Structural characteristics including presence of liver transplant program, bed capacity, teaching status, payer mix, staffing patterns also varied across hospitals (p< 0.01). Patient factors were significantly predictive of mortality including hepatitis C, alcoholic liver disease, portal hypertension, hepatorenal syndrome and co-morbidities (all, p<0.04). After adjusting for patient factors, there was nearly a 12-fold difference in mortality across hospitals (1.2% – 14.2%, p = 0.05). Hospital cirrhosis volume explained 10.4% of risk-adjusted variation in mortality. Liver transplant program status accounted for 13.9% of variation, however, payer mix, teaching status, ICU capacity, and staffing explained an additional 40.2% of variation in mortality between hospitals (Table 1).
Conclusions: There are tremendous differences between hospitals admitting cirrhotic patients and their outcomes. After accounting for patient differences, hospital structural characteristics account for 64.5% of the overall variation between hospitals. Cirrhosis mortality variation may be ameliorated by structural, programmatic, and process improvement.
To cite this abstract in AMA style:
Mathur A, Chakrabarti A, Sheetz K, Mellinger J, Volk M, Katariya N, Singer A, Hewitt W, Reddy K, Moss A. Hospital Characteristics Mediate Variation in Cirrhosis Mortality in Transplant and Non-Transplant Facilities [abstract]. Am J Transplant. 2015; 15 (suppl 3). https://atcmeetingabstracts.com/abstract/hospital-characteristics-mediate-variation-in-cirrhosis-mortality-in-transplant-and-non-transplant-facilities/. Accessed February 17, 2026.« Back to 2015 American Transplant Congress
