HLA Mismatching Does Not Have an Impact on Graft or Patient Survival in Simultaneous Kidney-Pancreas Transplantation. A Single Institution Experience.
Indiana University Health, Indianapolis
Meeting: 2017 American Transplant Congress
Abstract number: C231
Keywords: Graft survival, HLA matching, Pancreas transplantation, Rejection
Session Information
Session Name: Poster Session C: Pancreas and Islet (Auto and Allo) Transplantation
Session Type: Poster Session
Date: Monday, May 1, 2017
Session Time: 6:00pm-7:00pm
 Presentation Time: 6:00pm-7:00pm
Presentation Time: 6:00pm-7:00pm
Location: Hall D1
Purpose: There is conflicting data on whether the level and type of HLA mismatching (MM) has an impact on pancreas, kidney, or patient survival in SPK. It is also unclear whether HLA MM is associated with the incidence of acute rejection episodes in SPK. We hypothesized that the level of HLA MM and the type of MM (HLA A, B, DR) would not be associated with adverse graft or patient outcomes.
Methods: To test this hypothesis, we analysed clinical data on all (N = 248) simultaneous pancreas kidney transplants (SPK) performed between 2003 and 2014 at our institution to assess the impact of HLA MM on graft and patient survival and the incidence of acute rejection. Our immunosuppression protocol is anti-thymocyte globulin, steroid free maintenance with tacrolimus and sirolimus. Since 2006 we have added Rituximab as part of our induction protocol.
Results: Mean age of patients was 45 +/- 9 yrs; 58.7% were males; 91% were caucasians. A total of 29.2% of cases had either organ rejection over the study period. Zero MM (2.8%) ; 1-3 MM 20.5%; 4-6 MM 76.6%. Mean and median level of HLA mismatch was 4.29 and 5 out of 6. Class 1 and 2 PRA was 0 in 87.5% and 93.5% of cases. All cases with DSA present were excluded. Since immunosuppression (IS) can be confounding, we looked at the whole cohort and a subset of patients in whom the initial IS of SRL/TAC was not altered.
In the whole cohort, there was no difference in pancreas graft , kidney graft or patient survival with HLA MM (0-3 vs 4-6MM). In the SRL/TAC Cohort, there was a statistically insignificant higher pancreas and patient survival (but not kidney survival) despite a higher degree of matching. There were also no pancreas graft/kidney graft or patient survival differences with HLA-A, B, DR level of mismatching (0 vs 1 vs 2). Finally, HLA MM was not associated with of acute rejection including level of DR MM. 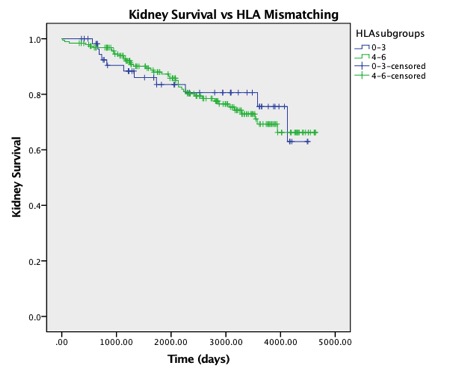 Conclusions: HLA mismatching in SPK at our institution using our regimen is not associated with an adverse impact on acute rejection, graft survival or patient survival.
Conclusions: HLA mismatching in SPK at our institution using our regimen is not associated with an adverse impact on acute rejection, graft survival or patient survival.
CITATION INFORMATION: Moinuddin I, Yaqub M, Taber T, Mishler D, Mujtaba M, Powelson J, Adebiyi O, Fridell J, Sharfuddin A. HLA Mismatching Does Not Have an Impact on Graft or Patient Survival in Simultaneous Kidney-Pancreas Transplantation. A Single Institution Experience. Am J Transplant. 2017;17 (suppl 3).
To cite this abstract in AMA style:
Moinuddin I, Yaqub M, Taber T, Mishler D, Mujtaba M, Powelson J, Adebiyi O, Fridell J, Sharfuddin A. HLA Mismatching Does Not Have an Impact on Graft or Patient Survival in Simultaneous Kidney-Pancreas Transplantation. A Single Institution Experience. [abstract]. Am J Transplant. 2017; 17 (suppl 3). https://atcmeetingabstracts.com/abstract/hla-mismatching-does-not-have-an-impact-on-graft-or-patient-survival-in-simultaneous-kidney-pancreas-transplantation-a-single-institution-experience/. Accessed February 27, 2026.« Back to 2017 American Transplant Congress
