HLA Broad Antigen and Eplet Mismatches in Determining the Risk of Acute Rejection After Kidney Transplantation
1School of Medicine and Pharmacology, University of Western Australia, Crawley, Western Australia, Australia
2Renal Medicine, Sir Charles Gairdner Hospital, Nedlands, Western Australia, Australia
3Nephrology, The Children's Hospital at Westmead, Sydney, New South Wales, Australia
4School of Medicine, University of New South Wales, Sydney, New South Wales, Australia.
Meeting: 2015 American Transplant Congress
Abstract number: 28
Keywords: Epitopes, Histocompatibility antigens, Kidney transplantation, Rejection
Session Information
Session Name: Concurrent Session: Kidney Antibody Mediated Rejection I
Session Type: Concurrent Session
Date: Sunday, May 3, 2015
Session Time: 2:15pm-3:45pm
 Presentation Time: 2:27pm-2:39pm
Presentation Time: 2:27pm-2:39pm
Location: Terrace I-III
Aim: To determine the clinical relevance of HLA-ABDR broad antigen and eplet matching for predicting acute rejection after kidney transplantation.
Background: HLAMatchmaker determines structurally HLA compatibility at the epitope level and may better predict the immunological risk of kidney transplants compared with broad antigen matching.
Methods: Donor-recipient broad antigen and eplet HLA-ABDR mismatches were calculated for all primary kidney transplants (n=3449) in Australia (2006-2011). Test performance characteristics of broad antigen and eplet matching for predicting acute rejection were examined using Receiver Operating Characteristic (ROC) analysis and net reclassification improvement (NRI).
Results: Of 3449 transplants with mean follow-up 3.6 (SD=1.8) years, 647 (19%) had acute rejection. There was a linear increase in the rejection risk with more broad antigen mismatches (p⟨0.001) whereby grafts with 5-6 mismatches was 90% more likely to experience acute rejection than grafts with 0-2 mismatches (OR 1.92, 95% CI 1.50-2.45). A similar association was present with eplet mismatches whereby grafts with ⟩20 HLA-ABDR eplet mismatches was 90% more likely to experience acute rejection than grafts with ⟨10 HLA-ABDR eplet mismatches (OR 1.89, 95% CI 1.4-2.56). Using broad antigen matching alone, the AUC of the ROC curve was 0.583 compared with 0.635 using a combination (Figure1). The NRI of rejection risk using eplet and broad antigen matching compared with broad antigen matching alone was -0.8% (p=0.408).
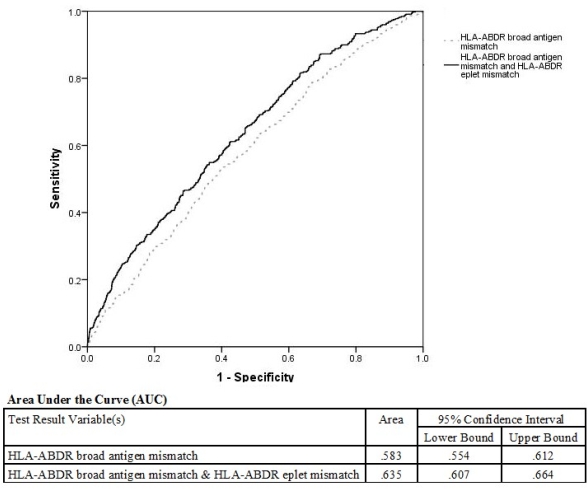
Conclusions: There was a linear association between risk of acute rejection and both eplet and broad antigen mismatch. The predictive accuracy of the model did not improve significantly with the addition of eplet matching compared to broad antigen HLA matching alone for predicting acute rejection in our cohort of kidney transplant recipients.
To cite this abstract in AMA style:
Nguyen HDo, Lim W, Chapman J, Craig J, Wong G. HLA Broad Antigen and Eplet Mismatches in Determining the Risk of Acute Rejection After Kidney Transplantation [abstract]. Am J Transplant. 2015; 15 (suppl 3). https://atcmeetingabstracts.com/abstract/hla-broad-antigen-and-eplet-mismatches-in-determining-the-risk-of-acute-rejection-after-kidney-transplantation/. Accessed February 23, 2026.« Back to 2015 American Transplant Congress
