Higher Hepatocellular Carcinoma Tumor Burden Score is Associated with Grater Liver Transplant Survival Benefit
1Surgery, University of Pittsburgh Medical Center, Pittsburgh, PA, 2Mathematics and Statistics, University of Arkansas at Little Rock, Little Rock, AR, 3Medicine, Medical Oncology, Yale University, New Haven, CT, 4Biostatistics, Massachusetts General Hospital, Boston, MA, 5Medicine, University of Pittsburgh Medical Center, Pittsburgh, PA
Meeting: 2022 American Transplant Congress
Abstract number: 1101
Keywords: Hepatocellular carcinoma, Liver transplantation, Organ Selection/Allocation
Topic: Clinical Science » Liver » 56 - Liver: Hepatocellular Carcinoma and Other Malignancies
Session Information
Session Name: Liver: Hepatocellular Carcinoma and Other Malignancies
Session Type: Poster Abstract
Date: Sunday, June 5, 2022
Session Time: 7:00pm-8:00pm
 Presentation Time: 7:00pm-8:00pm
Presentation Time: 7:00pm-8:00pm
Location: Hynes Halls C & D
*Purpose: Liver transplantation(LT) is the best treatment option for early-stage hepatocellular carcinoma(HCC) and cirrhosis. However, patients with various tumor burdens receive identical listing priority, despite the strong correlation between higher tumor burden and greater waitlist(WL) dropout risk. Our primary aim was to assess the effect of tumor burden score(TBS) on WL and post-transplant outcomes and transplantation-associated survival benefits.
*Methods: The Scientific Registry of Transplant Recipient(SRTR) was used to identify HCC patients listed for LT between 2002 and 2019. TBS was defined as the distance from the origin on a Cartesian plane incorporating maximum tumor size and the number of lesions. We used competing risk subdistribution hazard regression to calculate WL dropout risks, Cox Proportional Hazards regression with time-dependent variable, with and without mixed effects to calculate transplant-associated survival benefits.
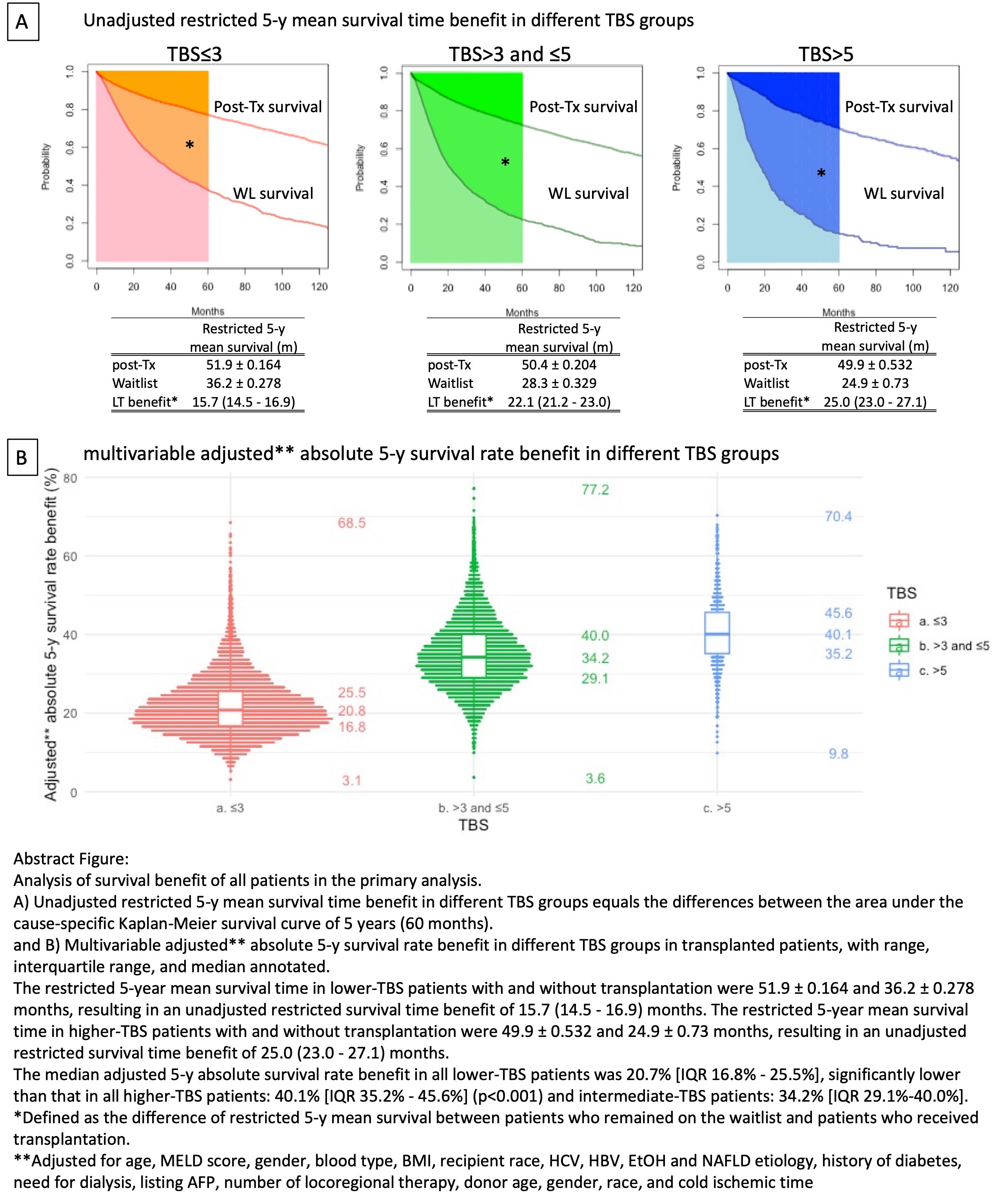
*Results: A total of 36,634 patients were included in the primary analysis, among whom 24,457 were transplanted. In competing risk analysis, Higher-TBS(>5) patients had a 52% greater relative risk for WL dropout than lower-TBS(≤3) patients. However, if transplanted, higher-TBS patients only have a 16% greater relative risk for death than lower-TBS patients. Additionally, LT yielded a greater risk reduction in overall death among higher-TBS patients (HR=0.237[0.201-0.280]) versus lower-TBS patients (HR=0.425[0.400-0.453]). Furthermore, transplantation provided higher-TBS patients larger survival benefits than lower-TBS patients: unadjusted 5-y restricted survival time benefit 25.0m(23.0-27.1) vs. 15.7m(14.5-16.9) (p<0.001) and median adjusted 5-y absolute survival rate benefit of 40.1%[IQR:35.2%-45.6%] vs. 20.7%[IQR:16.8%-25.5%] (p<0.001).
*Conclusions: HCC Patients with higher TBS waiting for LT have a greater risk for dropout and death than patients with lower TBS. Counterintuitively, their LT-associated survival benefit is superior to patients with lower TBS.
To cite this abstract in AMA style:
Liu H, Zhang W, Di M, Lee H, Cruz R, Wang X, Kaltenmeier C, Thompson A, Reddy D, Ashwat E, D'Alesio M, Lebowitz S, Tohme S, Geller D, Tevar A, Hughes C, Humar A, Behari J, Bataller R, Hariharan S, Molinari M. Higher Hepatocellular Carcinoma Tumor Burden Score is Associated with Grater Liver Transplant Survival Benefit [abstract]. Am J Transplant. 2022; 22 (suppl 3). https://atcmeetingabstracts.com/abstract/higher-hepatocellular-carcinoma-tumor-burden-score-is-associated-with-grater-liver-transplant-survival-benefit/. Accessed March 6, 2026.« Back to 2022 American Transplant Congress