Heart Transplant Outcomes in Adults with Peripartum Cardiomyopathy
Department of Cardiology, Keck Medical Center of University of Southern California, Los Angeles, CA
Meeting: 2020 American Transplant Congress
Abstract number: B-267
Keywords: Heart transplant patients, Heart/lung transplantation, Pregnancy
Session Information
Session Name: Poster Session B: Heart and VADs: All Topics
Session Type: Poster Session
Date: Saturday, May 30, 2020
Session Time: 3:15pm-4:00pm
 Presentation Time: 3:30pm-4:00pm
Presentation Time: 3:30pm-4:00pm
Location: Virtual
*Purpose: We aimed to evaluate long-term heart transplant (HT) outcomes in adults with peripartum cardiomyopathy (PPCM) and compare them to all other heart transplant recipients.
*Methods: The UNOS registry was queried for all cardiac transplants in the registry from 1987 to 2019 to compare characteristics and outcomes for PPCM-patients and all other HT patients. Variables including age, sex, diabetes status, ethnicity, ischemic time, dialysis, life support measures, days on waiting list and HLA-mismatch were used for multivariate Cox proportional hazard regression analysis. Survival curves were generated with the Kaplan Meier method.
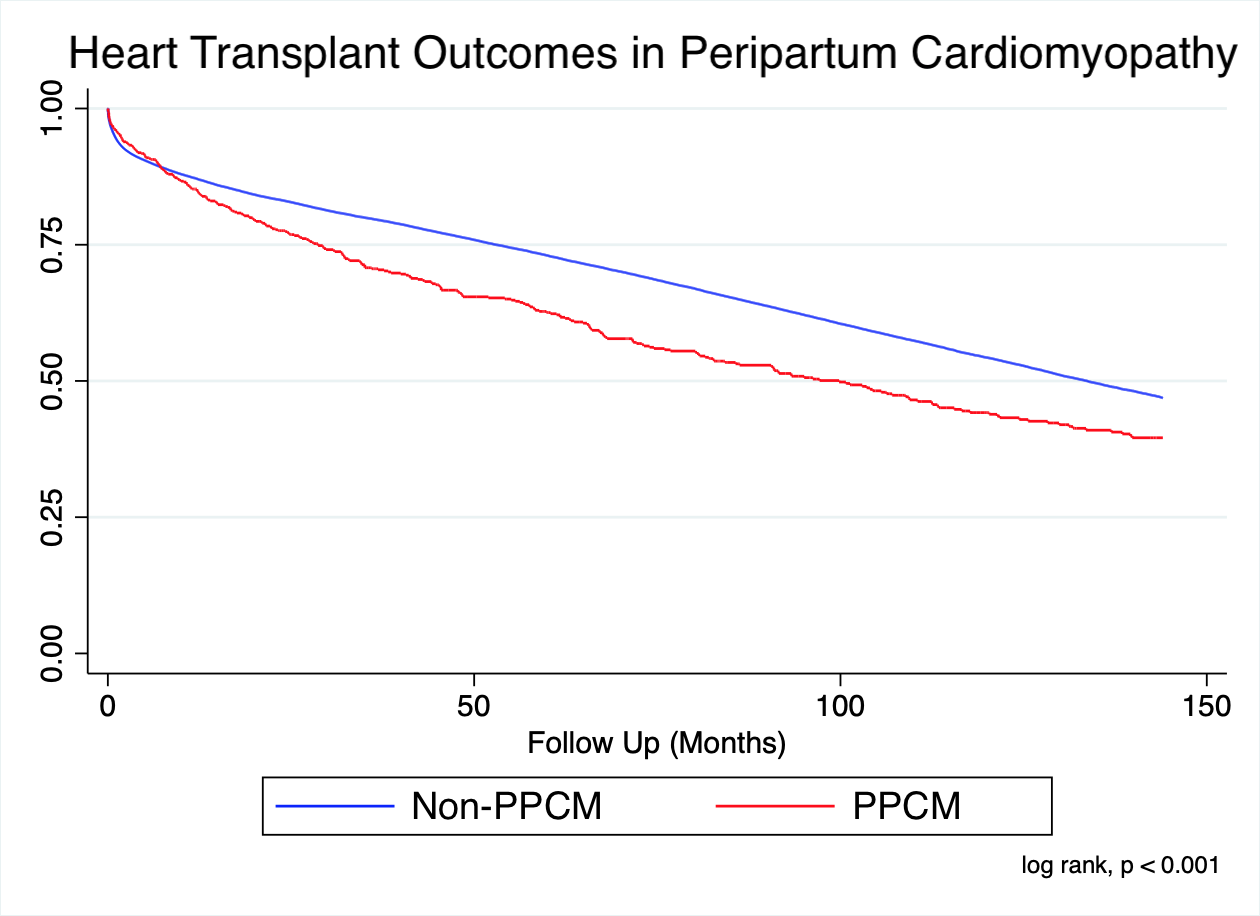
*Results: Between 1987 and 2019, 63,142 patients received a heart transplant. Of these patients, 666 women had a heart transplant in which the indication was PPCM. These patients tended to be younger (p<0.001), less likely to have diabetes (p<0.001), and less likely to smoke (p<0.001). About 48% of all PPCM patients requiring HT were African American. PPCM-patients were more likely to have required prior cardiac surgery (p<0.001) and higher frequency of support pre-transplant (p<0.001), including intra-aortic balloon pump (IABP) (p=0.006), ventricular assist device (VAD) (p < 0.001) but not extracorporeal membrane oxygenation (ECMO) (p=0.47). PPCM patients had fewer median days on the wait list prior to heart transplant (57.5 vs 83.0 days, p<0.001). In the PPCM group, there was significantly greater incidence of pre-transplant panel reactive antibodies > 20% (22.2% vs. 9.4%, p<0.001). The overall post-transplant survival was significantly lower in the PPCM group (Figure, p<0.001).
*Conclusions: Heart transplant patients with peripartum cardiomyopathy are more likely to be younger and with fewer chronic medical issues. However, they exhibit increased sensitization, increased use of life support measures and poorer survival outcomes after heart transplant compared to the general heart transplant population. Further investigation is warranted to better understand these findings.
To cite this abstract in AMA style:
Genyk P, Yang K, Liu G, Nattiv J, Banankhah P, Kingsford P, Li J, Nuno S, Pandya K, Vaidya A, DePasquale E. Heart Transplant Outcomes in Adults with Peripartum Cardiomyopathy [abstract]. Am J Transplant. 2020; 20 (suppl 3). https://atcmeetingabstracts.com/abstract/heart-transplant-outcomes-in-adults-with-peripartum-cardiomyopathy/. Accessed February 19, 2026.« Back to 2020 American Transplant Congress